Basal insulin Management in T1D
The Baseline of Insulin Management - Article 5 of 7 in Systems Approach Series
Overview
The current insulin regimen for glucose management is called basal-bolus, named after its two components:
- Basal—background insulin reflecting second phase insulin release from a healthy pancreas
- Bolus—prandial insulin for the first phase, meal-related, dose. “fast acting” Regular insulin was used for this in the past, but now it’s usually “rapid-acting” insulin Lispro or Aspart.
This manual implementation of the workings of a healthy pancreas is not just new, but probably the final glucose control strategy because of its attempt to recreate natural physiology. Effectively implementing Basal-Bolus management, however, remains an ongoing task that requires considerable work.
There are two notions of the purpose of basal insulin, both involving something “steady”:
- Steady insulin action all day long from, typically, one dose of insulin.
- Steady blood glucose (while fasting) resulting from a regimen requiring multiple doses of more than one type of insulin.
Steady insulin action
To achieve a basal insulin regimen that will produce steady insulin action all day long, one can use these insulins:
- Ultra-long-acting insulin Degludec (Tresbia)
- Long-acting insulins Glargine and Detemir
They are available in different concentrations and with different names, even at the same concentration. For example:
- Glargine is known as Lantus at 100 IU/ml and Toujeo at 300IU/ml, but also as a biosimilar named Basalin, and one named Basaglar, also at 100 IU/ml.
- Detemir is known as Levemir at 100 IU/ml and has roughly the same action time profile as Glargine. It has a biosimilar, too: Zarxio®
Insulin action
Glargine and Detemir have roughly 24-hour insulin action and are intended for once a day dosing. Deglucec lasts roughly 42 hours but is usually administered once a day as well. At 42 hours duration, at least a half day period somewhere between injections would be covered by both the previous and new dose, but either no one has noticed this, or the two to one variation in action for part of the day doesn’t bother anyone. It’s difficult to evaluate the effect of basal insulin action in any event, because that requires constant monitoring of glucose while fasting no less, the entire length of time the insulin is active. No one wants to fast that long, and the 24-hour insulins are, in practice, evaluated 12 hours at a time, moving the fasting portion around to evaluate each period, if they’re evaluated at all.
Hypoglycemia risk compared to NPH
After Glargine and Detemir were developed in 2002 and 2003, the first thing everyone wanted to know was how well they worked with regard to hypoglycemia. Many studies were made comparing them with the previous insulin used, intermediate-acting NPH. Unfortunately, the standard statistical technique for this (analysis of variance) determines how much of a “treatment effect” each alternative has. Thus there should only be a few to compare, but because there are many possible treatments using NPH, in number, timing, and dose, choosing one is problematic. Even the Glargine and Detemir treatments could be administered at different times of day, though that sort of shift, at least, had minimal impact.
When it came to choosing a specific treatment to compare, some researchers gave NPH just once a day, despite its action time of little more than 12 hours. The others all used it twice a day, as was done in the old split-mixed regimen. I could find no published papers that used NPH more than twice a day, though, with a six-hour peak effect and 12-hour action, three times a day would seem reasonable, at least to try. Medical research tends to evaluate standard operating procedure, however, and rarely looks into a more difficult or expensive possibility if it isn’t used.
In the 15 years since their development, some 200 studies have been made (typically paid for by the manufacturer) comparing Glargine and Detemir with NPH. They all found little HbA1c difference between them, though NPH was usually found to have slightly more frequent hypoglycemia. Hypoglycemia, per se, however, is a function of dose as much, if not more, than insulin type, so I don’t think ascribing this tendency to NPH itself is justified until carefully titrated NPH used three times a day has been evaluated. That sort of NPH “treatment” may well be better than the others, since it allows for different insulin sensitivity for each of three eight hour parts of the day, particularly relevant when one part has to accommodate the dawn phenomenon. Sadly, NPH has lost some marketing appeal due to these studies, a shame given its markedly lower cost compared to the less appropriate long-acting insulins. Moreover, no one has evaluated NPH in combination with Regular insulin in the tailored physiologic regimen I describe below.
Steady blood glucose concentration
The other understanding of a basal insulin regimen, one with steady glucose concentration while fasting requires some work, but I believe this is the only proper way to think of basal insulin.
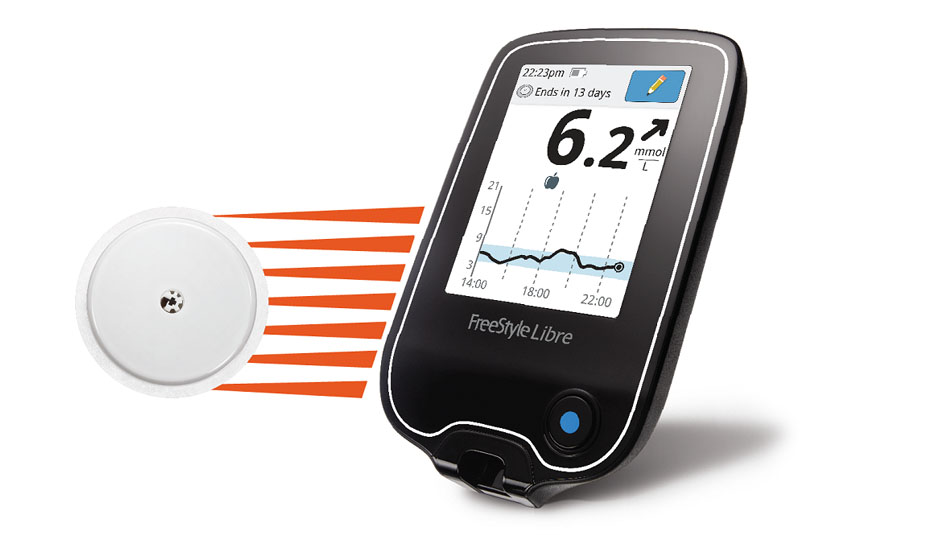
It is only since continuous glucose monitoring has been available that I have been able to investigate an insulin action profile for basal insulin. The insight I have gained from my CGM is that there really is no such thing as “basal insulin”, but rather a basal insulin action profile, implemented with CSII or MDI.
In CSII, the hourly infusion rate needed (to counter the dawn phenomenon) goes up around 5 am, climbs gently until about 8 or 9 am, then drops gently until 11 am when it falls back to the “basic basal” rate for the rest of the day. This basic rate can vary from afternoon to evening and overnight due to insulin sensitivity changing from different degrees of activity, but not by much.
With MDI, the basic basal insulin action can be achieved with each of three NPH doses, with the dawn phenomenon accommodated with two doses of Regular insulin, one at 5 am and another around 8 am. Alternately, this basic basal insulin action that only varies a little during the day may be satisfied by a single dose of 24-hour insulin. Not quite as perfect, but much less trouble. In my case, the two dawn related doses amount to roughly the same as the three basic NPH doses (or one ultra long-acting dose), with the total coming to the same as the usual formulas call for basal insulin overall (40-50% of total).
The total insulin need (of which basal is 40%) tends to depend on how much you weigh, though the underlying metabolism that contributes to that weight influences need as well. That need is easy to calculate in pounds: weight divided by four. Otherwise, its .55 times your mass in Kilograms.
Here is an example of the time, insulin type and dose for a body weight of 167 pounds, calling for just under 42 total units of insulin per day, and a basal need of 16 3/4 units:
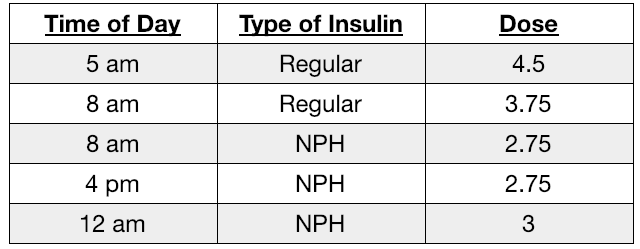
These doses and times are all subject to evaluation using CGM while fasting, ideally on different days of the week. Don’t just use these numbers, though, even if you weigh close to 167 pounds. My use of this (proportional) basal insulin profile with CGM shows glucose remaining within 20 to 30 mg/dl all day long, which is steady enough bolus insulin need remains unaffected.
In the section titled ‘Bolus Insulin Management’, we’ll discuss calculating the bolus dose (as today’s smart insulin pumps do). All of the formulas I’ve seen, both for insulin pumps as well as for bolus advice apps, and even the papers I’ve read, do not have a term for imperfect basal insulin. They all presume that the basal dose is just enough to keep glucose steady, and not trend up or down. It’s a presumption basal dose implementors should keep in mind, and because of the dawn phenomenon as well as variable insulin sensitivity during the day, something that requires variable basal insulin, rather than steady insulin action. So while many, if not most, physicians think of basal insulin as steady insulin all day long, the bolus formulas all call for it to have variable insulin action that, when done right, results in steady glucose all day long.
Acronyms and References
(see Master List)
|
Aspart |
|
|
Blood Glucose (aka BG) |
|
|
CGM |
|
|
CSII |
|
|
Degludec |
|
|
Detemir |
|
|
Glargine |
|
|
HbA1c |
|
|
Lispro |
|
|
MDI Multiple Daily injections |
|
|
NPH (aka intermediate insulin) |
|
|
prandial |
|
|
Regular insulin |
|
|
titrate |
Content of Series
There are six articles in the series plus a dedicated section on Acronyms and References.
- My T1D Journey as a Systems Engineer
- Physiology of Managing T1D
- Food Effect on Glucose
- Basal Insulin Management in T1D
- Bolus Insulin Management in T1D
- Using CGMs, Insulin Pens, and Pumps
- Acronyms and References
See description of full article series here.