Study Aims to Prevent Scarring from Infusion Sets and CGMs
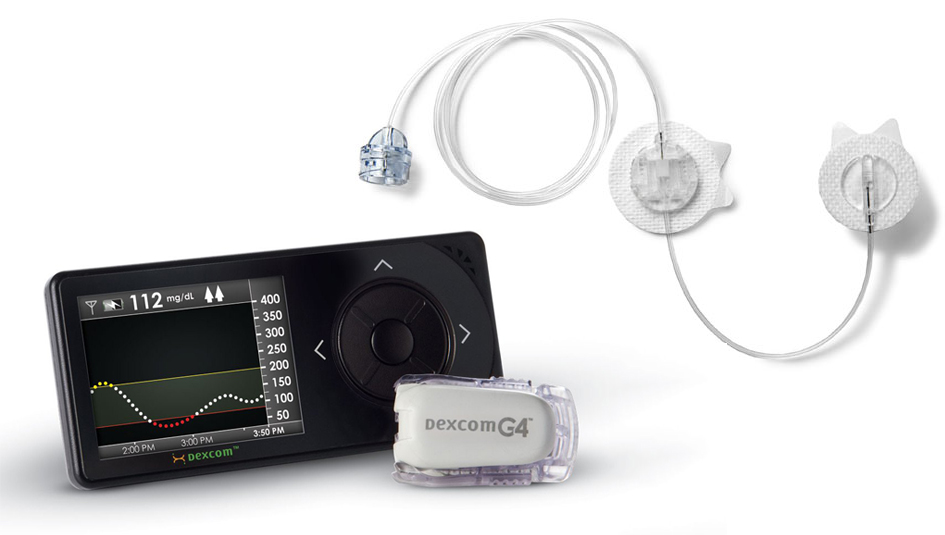
Researchers at MIT and Boston Children’s Hospital are trying to find ways to help the body’s immune system react less to materials used in implanted medical devices. The results of the study could have a significant impact on the quest to prolong the use of medical equipment for treating Type 1 diabetes, such as insulin pump infusion sets, continuous glucose monitors (CGMs), and cell encapsulation and transplantation devices.
The study focuses on how to control the body’s reaction to a foreign object in the skin. Researchers are trying to find ways to stop a protein known as CSF1R from creating an immune system response that could increase scarring and decrease the effectiveness of drug delivery and glucose monitoring. Researchers have found that when they administered the compound GW2580 to animal test subjects to neutralize CSF1R, it improved biocompatibility and reduced the thickening and scarring of connective tissue around an implanted device. This improvement was achieved without the need for administering a broader immunosuppression therapy that could inhibit other necessary immune system functions, like wound healing. The report was published in Nature Materials.
The process that researchers are trying to prevent is known as fibrosis. That’s when the immune system sends cells to create a barrier of scar tissue to border off the bloodstream from foreign contamination. This process is helpful when you have a splinter, but less so when it happens around infusion sets and CGM cannulas. That thickening and scarring can negatively impact the delivery of insulin and the accuracy of glucose readings.
Esther Latres, director of translational development at JDRF, found the initial results of the study promising. She also was pleased that the compound used to control CSF1R did not affect the immune system’s response for wound healing.
“This would allow for devices used in the treatment of Type 1 diabetes to be worn for longer periods of time (and to) perform their tasks more effectively,” she said. “The potential to prevent fibrosis could eventually lead to the development of implantable pumps or continuous glucose monitors.”
Initially, this research effort was more narrowly focused on trying to make better materials for islet cell transplantation, according to Julia Greenstein, JDRF’s vice-president of discovery research. However, when progress was made at neutralizing CSF1R, researchers realized their work could have wider ramifications for other tech-based therapies. Greenstein chalks it up to the “serendipity of science”
“We…came to the realization that hey, this could help other things like infusion sets, or even non-Type 1 devices that might be implanted, like hip replacements,” Greenstein said.
It should be noted that the study is still in the initial stages and has not yet been tested on human subjects, so it remains to be seen if the same techniques can deactivate the right parts of the immune system in the human body.
Thanks for reading this Insulin Nation article. Want more Type 1 news? Subscribe here.
Have Type 2 diabetes or know someone who does? Try Type 2 Nation, our sister publication.







