Are Immune-Evasive Islet Cells the Key to a Type 1 Cure?
Lab generated islet-like organoids produce insulin in response to rising blood glucose levels and can be transplanted without immunosuppressive drugs
Pancreatic and islet cell transplants have been used to cure diabetes in high-risk individuals. But, due to issues with availability and risks associated with immunosuppressive drugs, these procedures are far from common.
Recently, researchers at the Salk Institute have come one step closer to solving one of these problems with the development of engineered islet cells that can be transplanted without the use of immunosuppressants.
Their research brings the pursuit of a true, life-long type 1 diabetes cure, that much closer to reality.
The Problem with Traditional Islet Cell Transplants
The first human pancreatic transplant was completed in 1966. The recipient was a woman with diabetes who was on dialysis. While widely hailed as a success, the patient actually died a few months later.
Since then, full pancreatic and simple islet cell transplants have become safer and more likely to succeed. But these procedures are still relatively uncommon.
The reason for this is two-fold.
- Pancreases are famously difficult to harvest and require the organ to be in perfect shape for the procedure to even be attempted. In fact, less than half of cadaver pancreases are suitable for transplantation.
- Harvesting cadaver islet cells is less difficult but “curing” a person with diabetes requires more cells than can be harvested from a single donor. Most recipients will require islet cells from two or even three donors before they are able to come off of insulin therapy.
Usable islet cells are so rare that only a small percentage of people are ever considered for this procedure.
The most likely candidates to be considered are a) type 1s who struggle with brittle diabetes and suffer through uncontrollable and damaging highs and lows despite strict blood sugar management and b) those with extreme hypoglycemia unawareness.
But even for these people, the procedure does not come without risk.
- Like most organ transplants, islet cell transplants require the use of life-long immunosuppressive drugs. These drugs keep the recipient’s immune system from identifying the new cells as foreign invaders and attacking them.
- For people with type 1 diabetes, the role of immunosuppressants doesn’t stop there. These drugs are also used to keep the patient’s immune system from attacking the insulin-producing cells the same way it attacked and killed the person’s original pancreatic cells.
Because these types of drugs have dangerous side effects, including cancer, the benefits of the procedure have to outweigh these serious risks before it can be considered.
Creating Immune-Evasive HILOS
Overcoming the need for immunosuppressant drugs was the main focus of the Salk Institute’s researchers when they set out to engineer a new type of islet cell.
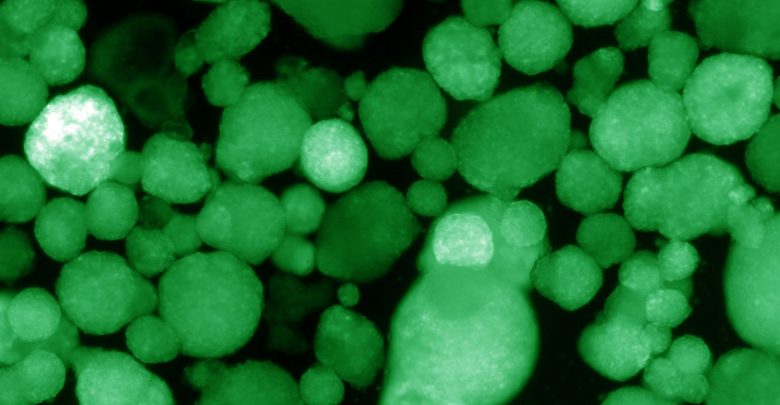
They were able to create human islet-like organoids (HILOs) from stem cells that were both robust enough to survive transplantation and that effectively produced insulin to maintain normal blood sugars.
Learning from Oncology
Once they had the beginnings of a successful islet cluster model they set out to make it invisible to the immune system using a trick borrowed from the field of oncology.
PD-L1 is a protein produced in excess by some cancerous cells that allow them to avoid detection by the immune system. PD-L1 inhibitors have been used successfully in immunotherapy treatments to fight these cancers.
The researchers took this knowledge and flipped it. By using short pulses of the protein interferon gamma they were able to induce their HILOs into expressing high amounts of PD-L1, effectively preventing immune rejection and T cell attacks.
The Next Steps on the Path to a Cure
A paper outlining the method of HILO creation and the successful trials of HILO transplantation in mice was recently published in Nature.
Expanded Testing in Mice
The researchers used the HILO approach to successfully cure diabetes in mice for 50 days without using any immunosuppressive drugs.
Now that the theory behind the research has proven to hold some weight, the researchers are planning to focus their energy on longer mice trials to determine just how long the HILOs will be effective in keeping blood sugars stable.
From there, the safe use of HILOs in humans will have to be established, at which point, human trials could potentially begin.
Can HILOs be Produced Efficiently?
But one major hurdle stands in the way of this potential treatment becoming a go-to cure for type 1: the availability and affordability of HILOs.
Like traditional islet cells, these specially engineered organoids are not easy to come up with. Current methods for their creation require removing the subject’s cells, regressing them into usable stem cells, and then engineering effective HILOs.
HILO production is a process that takes time and costs a substantial amount of money.
But if further studies into their use show promise, these researchers will have gotten closer to a feasible cure for type 1 diabetes than most others that have come before them.







