Glucagon the Sole Focus of a Bionic Pancreas Trial
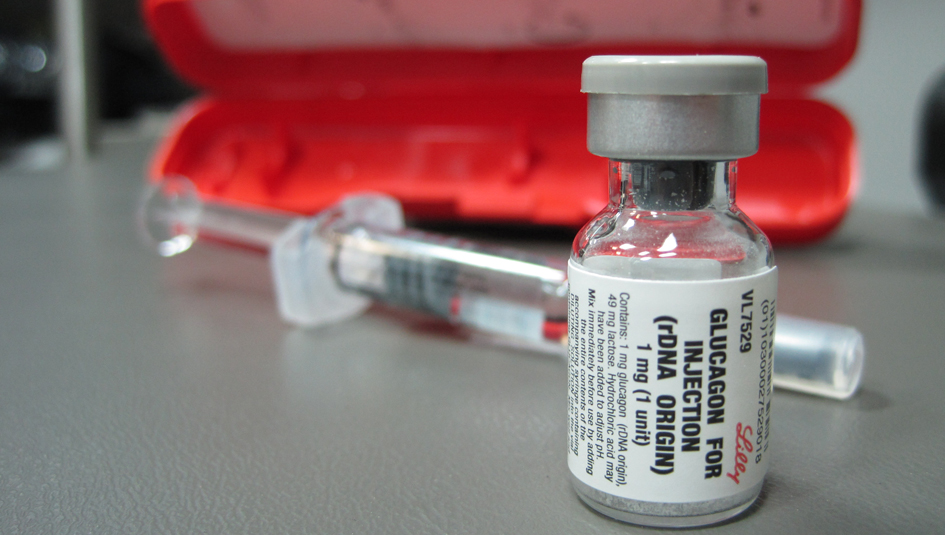
Glucagon – it’s not just for emergencies anymore.
That seems to be the growing sentiment among diabetes researchers as the treatment is being tested for use in a dual-chamber bionic (or artificial) pancreas and as pharmaceutical companies race to commercialize a version of the substance that is room-temperature-stable.
For the bionic pancreas to win FDA approval, it will need to prove that the novel aspects of the treatment are safe and effective. Recently, a team of researchers at the Massachusetts General Hospital Diabetes Center in Boston conducted a trial that focused exclusively on the automated delivery of glucagon to see if the treatment could prevent hypoglycemia and generally keep study participants in a desired range of blood sugar control.
According to a Healio Endocrine Today report, 22 adults with Type 1 were hooked up to bionic pancreas devices that only delivered glucagon or a placebo, not insulin. The participants used traditional methods (insulin pumps or multiple daily injections) to administer their own insulin. Researchers found that automated glucagon delivery cut the amount of time that blood sugar levels fell below 60 mg/dL by 75%, and cut the amount of symptomatic episodes of hypoglycemia in half. In other words, glucagon did its job to regulate everyday blood sugar swings and counter insulin.
And earlier this year, a Baylor College of Medicine study seemed to prove that mini-doses of room-temperature-stable glucagon were an effective way to treat minor bouts of hypoglycemia. Twelve adults with Type 1 on insulin pump therapy were given three small doses of glucagon from a pen being developed by Xeris Pharmaceuticals after their blood sugar levels had reached between 70 mg/dL and 74 mg/dL. Within an hour, the participants’ blood sugar levels had risen between 19 mg/dL and 43 mg/dL, depending on the size of the dose of glucagon administered, according to another Healio Endocrine Today report.
These are the kinds of trials that, while not flashy, are necessary to get FDA regulators to approve novel drug treatments. They lay the groundwork for making dual-drug therapy for treating Type 1 diabetes a real possibility.
Thanks for reading this Insulin Nation article. Want more Type 1 news? Subscribe here.
Have Type 2 diabetes or know someone who does? Try Type 2 Nation, our sister publication.







