Research Corner: Helping the Pancreas Help Itself

It is an exciting time for research into how to treat Type 1 diabetes. I and my fellow researchers at Perle Bioscience, as well as many other researchers, now understand that combining immunotherapy with new therapies discovered by using the Human Genome Project show great hopes of getting the T1 pancreas working again. But before we talk about where we’re going with T1 therapy, it might be helpful to review where we’ve been:
On the evening of October 31, 1920, when Dr. Frederick Banting scribbles on a piece of paper that clamping the pancreatic ducts in dogs may lead to a secretion that would help patients with diabetes.
Banting had just completed reading an article by Dr. Moses Barron on Islets of Langerhansas in patients who suffered from pancreatic stones that block enzyme secretion. Banting was struck by how the pancreas attempted to heal in reaction to injury. After reading the article, he hypothesized that collecting internal secretions of the pancreas, obtained by tying off the pancreatic ducts of dogs, would lead to a substance that might help patients with diabetes.
It may have been a eureka moment, but it wasn’t an easy path from thought to reality. Banting endured many failures in trying to prove this idea, and even had to sell his beat-up Ford to afford his last dogs for study. At last, he was able to prove that the secretions improved glucose levels in dogs. Soon he used his discovery to restore 14-year old Leonard Thompson, who had been on the brink of death from diabetes, back to health.
Of course, Banting’s secretions later became known as insulin. In many ways, this was the last great leap forward in diabetes treatments. Since then, new ways have been developed to acquire and develop insulin, but nothing has restored the pancreas to its normal state of functioning
There may now be another way forward, and it involves trying to tap into the powers of the pancreas to heal itself and get back to the business of making islets. In this field of research, we’re trying to add a new twist on an idea that has been known in scientific circles for almost as long as insulin. As far back as 1930, Dr. Geza de Takats declared in a paper that “regenerative powers of the pancreas were well known”. Dr. de Takats tied off the pancreas of children with diabetes in order to regenerate new islets, a procedure that had some success, but not enough staying power.
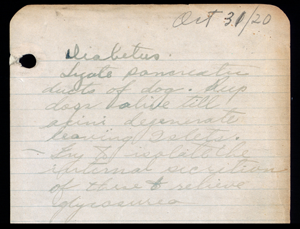
to himself about the possibility of manufacturing
what would become known as insulin.
We have known the pancreas can regenerate islets, but we’ve been lacking the genetic know-how to make such a treatment a permanent fix. Luckily, our knowledge of genetics recently has taken its own leap forward. By studying the work of not only Banting, Moses, and Dr. de Takats, our group is forming a new path of research, merging the work of the past with the work of the present.
The analytic tool we’ve been using is the Human Genome Project, an international scientific research project designed to study and identify all of the genes in the human body. A sample of blood or a swab from the mouth from a population of patients with conditions like Type 1 diabetes can help reveal what genes patients have in common that are different from the genes of the general population.
But instead of asking what genes patients with Type 1 or Type 2 have in common with each other, our team and other researchers have been asking what genes are expressed in acute pancreatic injury, like the kind found in Dr. Banting’s initial study. We found that the same genes are expressed when the pancreatic duct are tied in animals as during the new onset Type 1 diabetes in humans.
What is the gene? It’s a regenerative (Reg) gene that becomes present when there is injury to the pancreas. It’s also the same gene present in the pancreas during islet formation in the developing fetus. After the peak number of islets is reached within the first year of life, production of the Reg gene in pancreatic cells is slowed to prevent too many islets from being formed to protect against hypoglycemia. After fetal development, it is the beta cells within islets that fluctuate, expanding or contracting for patients to maintain their glucose within a very narrow range.
What researchers have proven in extensive lab tests is that this regenerative gene generates new islets from adult stem cells in the ductal tissue of the pancreas. The Reg gene has been shown in both animal models and in human pancreatic cells to regenerate new islets which contain all 6 hormones required to maintain glucose homeostasis (normality). One study showed that patients who had type 1 diabetes for 20 years experienced a 27% rise in C-peptides (a marker of one’s own pancreas making insulin again) with Reg gene therapy. And while this gene therapy may sound complicated and futuristic, it actually could even be delivered through an injection or, even possibly, by pill.
 Past efforts aimed at curing T1 involve suppressing an autoimmune attack on beta cells. We now know that Type 1 is not simply a disease of autoimmunity, but a disease of lack of beta cell regeneration. An effective cure or permanent therapy to restore homeostasis will require a one-two punch of stopping the body’s immune system from attacking the pancreas and helping the pancreas generate more islets. The beta cells within these new islets will need immune protection, but the possibilities for insulin independence are imminent.
Past efforts aimed at curing T1 involve suppressing an autoimmune attack on beta cells. We now know that Type 1 is not simply a disease of autoimmunity, but a disease of lack of beta cell regeneration. An effective cure or permanent therapy to restore homeostasis will require a one-two punch of stopping the body’s immune system from attacking the pancreas and helping the pancreas generate more islets. The beta cells within these new islets will need immune protection, but the possibilities for insulin independence are imminent.
As we look to the future of how we will one day cure diabetes, combining the knowledge of the past with the modern Human Genome Project may enable us to help the body help itself in ending Type 1 diabetes.
Thanks for reading this Insulin Nation article. Want more Type 1 news? Subscribe here.
Have Type 2 diabetes or know someone who does? Try Type 2 Nation, our sister publication.







