Advancements in Continuous Glucose Monitors (CGMs)
Part Two of a Series on Advanced CGM, Insulin Delivery, and Artificial Pancreas
Introduction
Diabetes is such a difficult condition to manage. With changes in your food, variations in exercise, stress, illness and a myriad of other factors that seem to change at random, it can be overwhelming. The good news is that this is one area in which technology can really help. Advances in Continuous Glucose Monitors (CGM), Insulin delivery systems and that holy-grail, the Artificial Pancreas can take away some of the challenges of managing all of these variables.
Diabetes technology companies have produced a dizzying array of new products that are all designed to help People With Diabetes (PWD) take better care of themselves. For those of you who want to peek under the hood at this tech, we have a series of articles just for you. These will each look closely at what technology is available now and what is coming down the road.
Article Series
Here is a summary of this series:
- CGM Sensors are good and getting even better (read article)
- Advancements in Continuous Glucose Monitors (CGMs) (this article)
- How does a sensor detect glucose?
- New CGM Technology on the Horizon
- Insulin Delivery Systems
- The Holy Grail, Artificial Pancreas systems
The articles on CGMs will look closely at what makes up a Glucose Monitoring System, get into detail on how glucose sensors actually work and look at some of the exciting and innovative devices on the horizon. The piece on Insulin Delivery Systems will look at pump technology, pen injectors, how they work and what new tech is coming down the pike. Finally, we will look at the Artificial Pancreas devices, what they are, how they work and when you can get one.
Why CGMs are so important?
A hallmark of Diabetes, especially T1D, is that it is one of the only chronic ailments in which the main treatment is education and tools to help a person manage his or her condition.
Study after study has shown that the more a person is able to keep his or her blood sugars within the normal range, the more likely they are to avoid the complications that we all hear about. The reason why this is so important is that when a person’s red blood cells are exposed to high glucose level they can cause damage to capillary walls. So, the organs that have lots of capillaries are most likely to suffer the most damage, such as the eyes, kidneys, and extremities. The good news is that by monitoring blood sugar closely, a person has an opportunity to take action to stay within range. This is not an easy task for sure, but knowing how your body reacts to food, exercise, stress, and illness gives you a fighting chance to steer clear of these nasty complications.
A CGM typically will monitor the blood sugar automatically every 5 minutes. Modern systems can supply this information in a way that is very easy to read, sometimes as easy as just glancing at a display. The easier it is to see the glucose level, the more often people will read it. The more often the glucose level is read the more often people will take action to keep it normal. The more often people take this action, the more they will stay free of Diabetic damage.
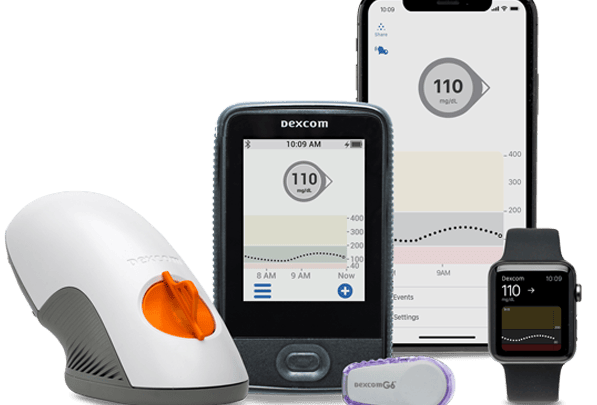
What makes up a Glucose Monitoring System
A CGM is much more than a pretty sensor. In order to be truly useful, a system needs to deliver a person’s glucose information when and where it is most needed. This could mean it is displayed on a person’s smartphone, on a watch, on a caregiver’s App, or provided directly to a physician. Here is a diagram showing how a glucose value can travel through the system.
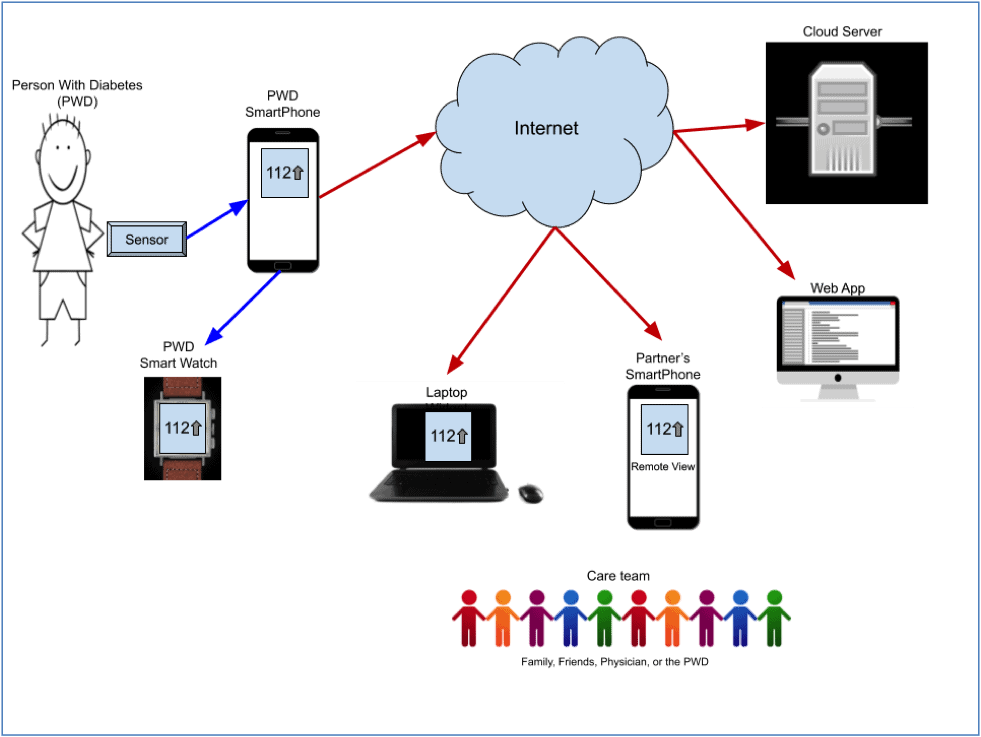
In this system, the sensor measures the Person With Diabetes’s (PWD) glucose then sends it to an App on the Smart Phone (using Bluetooth) where the PWD can view the reading. From there the value can be sent to the person’s watch so it can be read more quickly just with a turn of the wrist. To get even easier, a widget can be installed on a Laptop where the value is constantly displayed and can be viewed with a quick glance of the eyes.
The phone forwards the value through the Internet to a Cloud Server where it is saved into a secure storage system. If the patient’s partner has a SmartPhone running a remote-view App, then the value can be automatically downloaded so that the partner can be alerted if the PWD falls into hypoglycemia. Finally, the PWD can sign up with web-based App services such as Glooko or Tidepool that will integrate the CGM data with insulin administration, exercise and even food consumption. All of this data can then be viewed by the PWD and/or the care team to truly see the relationship between what a person eats, how they exercise, how they take insulin and their blood sugar. With this full understanding of how the Diabetic’s body really works, they have a fighting chance to keep their blood sugar under control.
Sensors
The vast majority of CGM sensors use an enzyme to help detect glucose in a patient’s body.
For those who have forgotten most high school chemistry, an enzyme is a protein that acts as a catalyst to speed up chemical reactions. The most common enzyme used in CGMs is called Glucose Oxidase, or GOx for short. Enzymatic sensors work with a small battery-operated computer to measure glucose. This works through a simple and usually reliable process.
In order for the sensor to work, a tiny electrode needs to make physical contact with the patient’s glucose. As you know by now, glucose is the body’s main fuel. When carbohydrates are digested, the stomach converts them to glucose and drops them into the bloodstream. With a proper amount of insulin, these sugar molecules can gain access to the red blood cells and provide fuel for the body’s functions.
Interestingly, because of their small size, glucose molecules naturally diffuse out of the capillaries into the surrounding area. This space contains fluid and is thus called Interstitial Fluid or ISF. This is great because it means that a CGM sensor can detect glucose without entering the bloodstream. A tiny electrode is inserted through the skin, usually about 1/3 of an inch, deep enough to contact the ISF.
The tip of the electrode is covered with the enzyme. After it has been inserted into the ISF, the computer in the sensor turns on a very low voltage circuit. If there is glucose in the ISF surrounding the sensor, then current will flow through the electrode. The computer can then measure the flow of current through the electrode. Since the amount of current flowing is proportional to the amount of glucose, the computer’s algorithm can use this information to estimate the sugar level.
Receivers & Apps
While not a sexy as sensors, receivers, Apps and Watches that can display a person’s glucose value play a key role in the Glucose Monitoring System. The best sensor in the world is not worth much if the glucose value can’t be seen by the people who need it. The first step in making this happen is to get the sensor connected to a Smartphone (using Bluetooth). In addition to displaying the glucose value on the screen, the phone can relay this information out onto the Internet, where there is a whole world of support available. The value can be stored on an Internet cloud server and from there distributed to the care team. A family member or friend can install a Remote View app to provide them with nearly instantaneous updates on the PWD’s glucose control. Alerts and alarms can be set up so that a caregiver is notified when values get too high or too low. This can be invaluable by providing another pair of eyes, another brain to help manage this crazy illness.
Research has shown that the more frequently a Diabetic reads his/her glucose value the more time they spend “in range”. This is simply a matter of reaction time and awareness. If a person’s glucose level gets out of control, it will tend to stay out of control until action is taken (insulin, exercise, etc). If the time between when the glucose rises and when it is noticed is shortened, then it is MUCH easier to get back in range.
Personal Reflections
Better access to CGM data has certainly been helpful to me. When I first got Diabetes, I used a Blood Glucose Monitor (BGM) which required me to prick my finger to determine my sugar level. In the best days, this happened 5-6 times a day, even though my glucose varied widely due to food, exercise (or the lack thereof), stress, illness and a myriad of other factors. Then I got a CGM with a receiver that I could carry in my pocket. Now whenever I wanted to see my glucose level, I could pull out the receiver, turn it on and see the level. Next step was to ditch the receiver and install an App on my phone and a Remote View App on my family’s SmartPhones. This further reduced the time between a glucose excursion and when it was noticed. Next step was a SmartWatch, which made it even easier. Now all I had to do is lift my watch to see the sugar level. This meant that I was able to see my glucose level very frequently and stay in much better control. Finally, (as if lifting the wrist was too much work) I installed a “widget” on my laptop. This little software application displays the glucose level constantly in the menu bar of my computer. All I have to do is lift my eyes from the keyboard to know instantly if I am in control, falling to hypo territory or rising and in need of insulin. You really can’t get much easier than that!
You may think that I am just lazy and reluctant to go through the hassle of pulling out my phone or even just lifting my wrist. While you may be right, the fact remains that having my glucose levels so readily available all time has given me an early warning system and the information that I need to manage my diabetes and has kept me complication-free for over 26 years.
Wrap Up

I hope you found this helpful. Diabetes technology can be extremely helpful in managing this crazy disease. Tech can be confusing and scary for some, so I hope this series will demystify it and show you how it can be helpful.
In the next article, I will really look under the hood to tell you how glucose sensors work.
I am always interested in feedback.
Tom Bishop Bishop MedTech Consultants, LLC https://www.bishopmedtech.net/ https://www.linkedin.com/in/tombishop/ eMail: tbishop56@icloud.com