A Cure Out Of Thin Air?

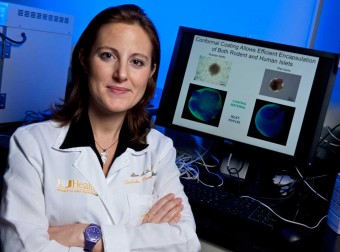
(left) Dr. Chris Fraker, DRI research assistant professor of surgery and cell transplantation (at microscope), with Vita Manzoli, senior research associate and member of his team.
Oxygen. It’s all around us — in the air we breathe, in the water we drink and, of course, in our bodies. Most people never think about the importance of oxygen to the function of their organs. But for scientists experimenting with novel methods of islet cell replacement therapy at Miami’s Diabetes Research Institute (DRI), having enough oxygen, where you need it, when you need it, is a critical part of making islet cell replacement — and a possible cure — more available for people with Type 1 diabetes. Islets, which contain the insulin-producing beta cells, consume nearly a quarter of the oxygen that flows through the pancreas, even though they comprise only one to two percent of the entire organ. And when donor islets are transplanted into a person with diabetes, the islets have a mortality rate of close to 80 percent due to several factors, one of which is inadequate oxygen supply.
Islet cell transplantation was first performed successfully in the U.S. in 1985 at the Diabetes Research Institute at the University of Miami and at Washington University in St. Louis, MO. A few years later, the automated method of islet isolation, invented by Dr. Camillo Ricordi, now DRI scientific director, dramatically increased the number of islets obtained from a donor organ. Over the years, there have been steady improvements in islet transplantation due in large part to the development of new anti-rejection drugs and better techniques and equipment. Many patients who have received islet cell transplants have been living insulin free for years or have greatly reduced insulin requirements, and an overall improved quality of life.
However, islets are hard to come by. Right now, researchers rely on donor organs, but the number of usable pancreases available in the U.S. is extremely limited — on average only about 1,700 per year — hardly enough to cure millions living with diabetes. While many strategies are under way to increase the supply of insulin-producing cells, the main priority now is to maximize the current supply by making every islet count. Toward this end, researchers have learned much about what is needed to keep islets healthy and happy and one of the key factors is providing them with an abundance of oxygen.
Christopher Fraker, Ph.D., is one of the DRI scientists crafting solutions to these problems, which begin with a mismatch of supply and demand. There are simply not enough islets available from human donors to match the need in basic research, much less for transplantation into patients.
“That’s why I do a lot of my early research using an immortalized cell line from mouse pancreatic tumors,” Fraker says. “They have some similarities to human beta cells and they just grow and grow.” Nonetheless, you can only learn so much about curing a disease in human beings by working with cells from mice.
Pigs are like people
“The lack of human islets steers us to pigs,” Fraker said. “The advantage is that their insulin structure is only one amino acid different from that of humans. Pig insulin was used to treat diabetes effectively for years before human insulin was available. The tough thing about pigs is that they’re a different species, and that makes transplantation very difficult. Now there are groups developing humanized pigs. They’re still pigs, of course, but their islets are more human, and the insulin they’re making is structurally the same as human insulin.”
Islets, which contain the insulin-producing beta cells, consume nearly a quarter of the oxygen that flows through the pancreas.
Long-term, Fraker is betting on the use of human stem cells – cells that don’t involve xenogeneic (cross-species) transplantation and are in plentiful supply. “You can guide stem cells in almost any direction,” he explained. “If you’re looking for a specific type of cell with specific features, you can develop a protocol. Once you have a protocol that works, you can scale up and almost mass produce them.”
Current sources of human stem cells, Fraker noted, include those from embryos and umbilical cords – even adipose tissue from liposuction procedures. “Cells from the individual patient might actually be best,” he said.
But stem cells destined to be islet cells need a rich oxygen supply to survive in the lab, as well as in the patient. Moreover, all islet-like stem cells go through a process called “terminal differentiation,” in which they become cells that produce either insulin or another hormone called glucagon, which the body uses to raise very low blood sugar. Undifferentiated precursor cells are vulnerable to immune attack when transplanted, just like fully differentiated islets, and in current protocols, terminal differentiation is performed in vivo (in the patient’s liver), where it can take up to three months after transplantation for them to develop into functional insulin-producing tissue. If that differentiation process can be accelerated in vitro (in the lab), the cells can go to work right away and be less vulnerable to rejection.
 The DRI’s answer is a patent-pending device they call the “oxygen sandwich.” It’s a culture dish whose normally impermeable plastic bottom has been replaced by permeable silicone rubber with perfluorocarbon mixed in. Cells in a liquid culture medium sit on the dish bottom, which, because it is permeable, allows oxygen to move up instead of down, as would have been the case in the traditional top-to-bottom diffusion method. The result? Much better oxygenation and more efficient differentiation, not to mention higher production of insulin and other hormones.
The DRI’s answer is a patent-pending device they call the “oxygen sandwich.” It’s a culture dish whose normally impermeable plastic bottom has been replaced by permeable silicone rubber with perfluorocarbon mixed in. Cells in a liquid culture medium sit on the dish bottom, which, because it is permeable, allows oxygen to move up instead of down, as would have been the case in the traditional top-to-bottom diffusion method. The result? Much better oxygenation and more efficient differentiation, not to mention higher production of insulin and other hormones.
Fraker foresees another potential benefit, although it’s currently his own unproven hypothesis. One problem with stem cells is the potential formation of tumors through uncontrolled growth. He believes that better-differentiated cells may prove less likely to go down that path. In addition, he noted, “Evidence shows that diabetes has a better response to more physiologically-differentiated cells. The better the response to glucose, the better the control of blood sugar levels.”
In a standard culture device, like a petri dish, oxygen is only diffused to the cell(s) from above (shown as O2 in the diagram) with the cells resting on the bottom, non-porous surface. Since oxygen is critical during islet cell development, the DRI invented the “oxygen sandwich,” that provides the vital oxygen to cells from the top and the bottom, similar to the native pancreas. To further maximize the available oxygen, the cells are placed on a silicone material that incorporates perfluorocarbon (PFC), an oxygen- binding material.
It’s personal
Fraker, like many of his co-workers, has a personal investment in his work. Diagnosed with Type 1 diabetes at age 16, he now has two daughters with the genetic markers for the disease. He said the kids with diabetes who come into the DRI for treatment provide his strongest motivation for continuing to push hard toward a cure. That and, of course, the DRI’s global connectivity to other research being conducted in and out of the diabetes arena.
Stem cells destined to be islet cells need a rich oxygen supply to survive in the lab, as well as in the patient.
“Working here is inspiring,” Fraker said. “We have telescience capabilities whereby we can see procedures elsewhere in the world as they are being performed. We’re also linked with scientists in other fields, such as cancer research. Cancer cells have ways to mask their presence so the body doesn’t recognize and destroy them, and learning how that works is of interest to us, too.
“One thing all of this interconnected research demonstrates,” he continued, “is that the immune system is very complex. As research progresses, it becomes more clear that a lot of these diseases are linked to one another, possibly caused by different environmental factors like diet and pollutants.”
Fraker began his career developing implantable glucose sensors, but he soon realized he wanted to conduct research that was more cure-focused. “I found the place doing the best and brightest work, and I kept chasing Dr. Ricordi until he offered me a tour and a job,” he recalled with a laugh. That was 14 years ago, and even the research avenues that turned out to be dead ends haven’t diminished his enthusiasm. “There is no such thing as bad data,” Fraker said. “You always learn something. Working here is like working on a giant puzzle, and every day you go in excited to find the solution. If you don’t, you try something else.”

Thanks for reading this Insulin Nation article. Want more Type 1 news? Subscribe here.
Have Type 2 diabetes or know someone who does? Try Type 2 Nation, our sister publication.