Is Newer Insulin Worth its Steep Price-tag?

Dr. David C. Robbins, director of the KU Diabetes Institute at the KU Medical Center, picked an auspicious place to suggest that we lack evidence to determine whether newer diabetes treatments are better diabetes treatments. After all, his talk on the subject, part of a panel discussion on rising insulin prices, took place during the 77th ADA Scientific Sessions, a conference where pharmaceutical company representatives showed off the latest diabetes technology and advocates listened eagerly to trial data to see what new treatments may come next.
At the beginning of his presentation, Dr. Robbins said it was difficult to prepare a talk on the possible value of older diabetes medications because there is little reliable data to share about these medications. Many of the clinical studies done on older treatments are too dated to be of use, and there are few head-to-head clinical trials between older generation treatments and newer ones, he said.
“The more I got into this, The more I realized that the data that we have to guide us in the use of these older medications compared to what we have now has been distorted, I think, by the marketing forces that have been around us,” he said.
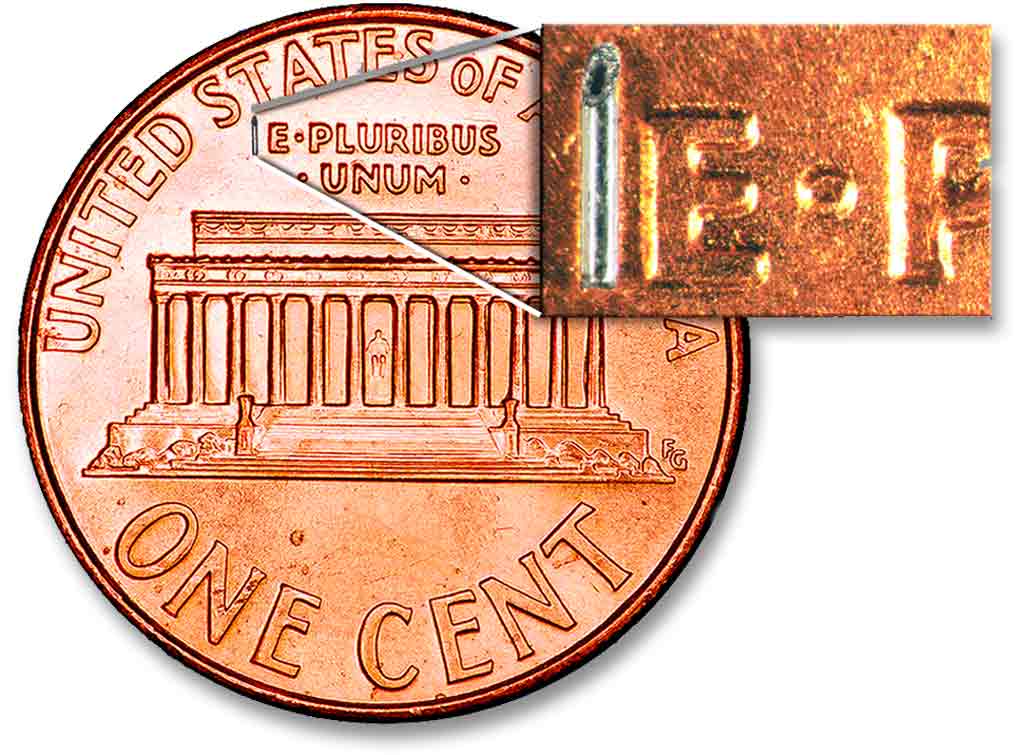
The lack of good data makes it harder for doctors to evaluate whether older, cheaper treatments might be good for some patients, he said. As an example, he asked for a show of hands of who in the room knew how to use NPH insulin for what he called “a poor man’s basal” insulin; no one raised their hand.
Another example that Dr. Robbins gave, one which he said he knew would be controversial, is urine testing for glucose levels. He cited an 18-month study in the early days of blood strip testing that found that there was no significant difference in glucose control between a group of patients using urine testing and another using blood-based test strip. Dr. Robbins said he knew that discussing this was tantamount to heresy, but he felt the question needed to be raised.
“There has not been adequate or fair head-to-head testing of the two methods,” he said.
Dr. Robbins’ comments have been critiqued by some in the diabetes community as a tonedeaf call to use older diabetes treatments, but a review of his presentation found he only called on the medical community to demand better evidence on the effectiveness of older diabetes treatments. He stopped short of advocating for any one treatment over another.
“We have to distinguish between ‘significantly better’ and ‘clinically important,’” he said.
This interpretation of his talk is strengthened by placing his presentation in context with the other speakers on the panel who were discussing the impact of high insulin prices. An earlier presenter shared an anecdote of a patient with diabetes who had an alarmingly high A1C score; the patient could no longer afford his top-of-the-line insulin and the presenter wondered if the patient’s health would have been better served if she had prescribed over-the-counter insulin earlier during the course of treatment.
During much of the rest of the talk, Dr. Robbins argued that doctors bear a sizeable amount of the responsibility for the rising price of drugs. Doctors often think they are immune to marketing efforts, but that their colleagues are not, he said. He called on doctors to be more honest about their susceptibility to marketing efforts.
“We are subject to market forces and innate motivations that are not always based in logic and fact,” he said. “We are all human and subject to conflicts of interest.”
He then spoke of a time in his career when tuition for his children’s schooling was more than his base salary as a doctor. To cover costs, he turned to giving talks sponsored by drug companies. At these talks, he dreaded being put into a position to actually say whether a drug was better or not than others that exist, for fear of either angering his sponsors or being untruthful.
He also listed common marketing traps that cause doctors to prescribe more expensive drugs. These included misplaced sentiments like a sense of obligation after a drug-company-sponsored event and a desire to want to give a patient the newest treatment out of an assumption it is the best, he said.
“I’m going to say, ‘We share the blame. We are part of the problem,’” he said.
Concluding his talk, Dr. Robbins called on doctors to demand better evidence of the efficacy of all diabetes treatments, new and old. He also briefly called on organizations like the ADA and medical journals to be more transparent and ethical about their funding from drug companies. He also briefly called on well-informed patients to do even more to educate themselves about treatments.
Do you have an idea you would like to write about for Insulin Nation? Send your pitch to submissions@insulinnation.com.
Thanks for reading this Insulin Nation article. Want more Type 1 news? Subscribe here.
Have Type 2 diabetes or know someone who does? Try Type 2 Nation, our sister publication.