Why Insulin Coupons & CoPay Caps Aren’t Good Enough
Novo Nordisk, Sanofi, and Eli Lilly reacted to insulin pricing outrage with modest and self-serving PR programs that do little; CMS is looming

Despite several years of activism, debate, and protesting, the biggest pharmaceutical manufacturers of insulin — Novo Nordisk, Eli Lilly, and Sanofi — have still not lowered the list price of insulin. Worse, the latest round of “insulin copay price caps” they have unveiled actually benefit these corporations financially.
Prices Skyrocket and Shareholders Benefit
The price of insulin in the United States has sky-rocketed more than 1000 percent since the late 1990s. Until recently, there has been no substantial action taken by the U.S. government to put an end to this price gouging.
Research from the University of Pittsburgh provided evidence that the net price of insulin in the United States had also soared – by 51% between 2008-2017. This is the price received by Novo Nordisk, Eli Lilly, and Sanofi.
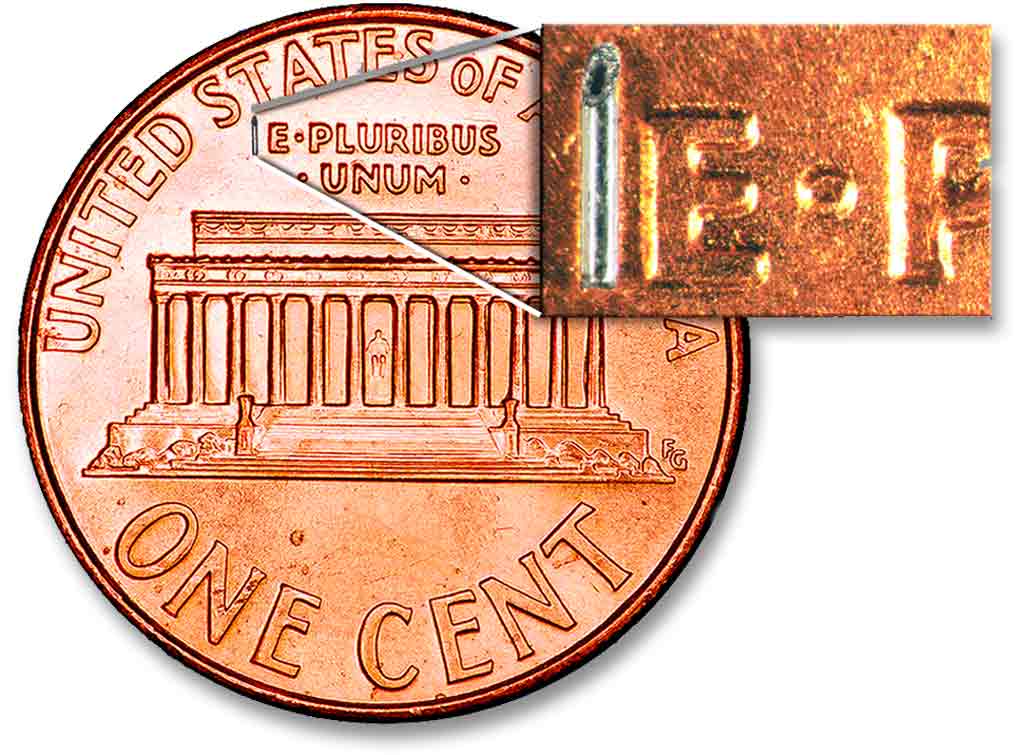
One vial of insulin costs a few dollars to produce, yet costs $320 for a patient in the United States and only $30 for a patient in Canada, explained Marina Tsaplina and Nicole Smith-Holt, both fervent advocates behind the #insulin4all initiative.
“The three insulin manufacturers have raised their prices in lockstep for many years now, prompting a class-action lawsuit and criminal investigations into collusion,” wrote Smith-Holt in her 2018 article for TruthOut. “Additionally, the insurance industry is also complicit in the drug pricing scheme.”
The Institute for New Economic Thinking published a report in April saying ‘Contrary to pharmaceutical company claims, revenue from high insulin prices are going to shareholders, not R&D.’
Will CMS Action Matter?
In March, the Trump Administration announced it was working to lower insulin prices for senior citizens on Medicare. While seniors are a mere fraction of the population of people with type 1 and type 2 diabetes who depend on insulin, it is a step in the right direction.
“Today, the biggest payer for medicines — the United States government — is legally prohibited from negotiating for the price of medicines with manufacturers. This means the industry can charge whatever they want,” added Tsaplina, “and they do.”
Breaking News — On May 26, 2020, the Centers for Medicare & Medicaid Services (CMS) announced a Senior Savings Model in which insulin copays will be capped at $35/month beginning in 2021. See the last section of this article for details.
#insulin4all and its work on the price of insulin
First launched by the founder of T1International, Elizabeth Pfiester, #insulin4all is a patient-led movement that doesn’t actually belong to any single organization or person but to everyone on the planet who needs insulin.
“It’s really a global call and cry,” explained Tsaplina, “and has become the tip of the sword of the medical crisis in the United States because the violations of insulin pricing in this country are so egregious and so obvious.”
Before the birth of #insulin4all, T1International operated as an international nonprofit organization committed to helping people across the globe with diabetes get the insulin they need to survive.
Unlike many advocacy organizations that rely on funding from BigPharma to keep their doors open and operations underway, T1International has steadfastly resisted this approach to funding.
“T1International accepts no funding from the pharmaceutical industry,” explained Tsaplina, “and is uncompromised in terms of industry alliance.”
When fighting for access to affordable insulin, this discrepancy in an organization’s source of funding is critical. Tsaplina knows this influence personally. She founded and directed a nonprofit that accepted industry funding. She writes that the influence of industry “is often revealed by what is not said.”
The #insulin4all initiative has led the way in exposing the pharmaceutical industry’s deceptive and greedy price gouging on insulin — the hormone all people with type 1 diabetes and many of those with type 2 cannot survive without.
The Problem with Insulin Copay Price Caps
The first “insulin copay price cap” bill was announced in Colorado with a $100 maximum expense to the patient no matter how much insulin they needed. Quickly, many patients discovered this new bill didn’t apply to them because of various exemptions in their health insurance plan.
The three big manufacturers of insulin did not offer their own price cap programs until this bill that they lobbied heavily against was passed in Colorado.
Shortly after national stay-at-home orders due to COVID-19 were issued, Eli Lilly seized the opportunity to appear generous by presenting their own “copay price cap” program that would cap insulin expenses at $35 per month for some patients.
Novo Nordisk followed shortly after by offering “free insulin for up to 3 months” for anyone who has lost insurance coverage related to COVID-19.
Over a year ago, Sanofi offered to limit insulin expenses for patients paying with cash to only $99 per month which completely ignores the still outrageous prices patients with health insurance face.
But Tsaplina and Smith-Holt point out that they still haven’t been required to lower the list price of insulin in the United States, which means they still aren’t concerned about a patient’s ability to afford insulin, making these price caps really just one large PR opportunity.
“I asked health insurance companies in Minnesota if premiums for health insurance plans would rise to compensate for the price caps on insulin, and they said it would not result in higher premiums,” explained Smith-Holt. “But we all know they’re going to need to recoup that money somehow in order to continue profiting.”
“Ultimately, these companies are really smart because when they do this, it’s a write-off for them as a charitable contribution and it’s a business loss that they can claim on their taxes,” said Smith-Holt.
“And they don’t even pay taxes, they actually get refunds of billions of dollars. It’s not a loss to them, they gain positive PR, good samaritan points, they gain a tax write-off, and they turn around profit from it off the federal government.”
Novo Nordisk, Sanofi, and Eli Lilly aggressively fought ‘Alec Smith Affordable Insulin Act’
In 2016, Smith-Holt’s son began rationing his insulin. No longer eligible to be on his parents’ health insurance plan, Alec died at the age of 26 from diabetic ketoacidosis — just two years after his type 1 diabetes diagnosis.
“He didn’t have insurance through his work,” explained Smith-Holt. “They were a small family-owned business that was not required to provide benefits such as insurance. We looked at purchasing insurance through the marketplace for him but based on his income and family size of ‘1’ the premiums were high at $450 a month with a very high deductible, like $7600, so he chose to not purchase the policy.”
As a healthy adult male, Alec would easily need at least 2 or 3 vials of insulin per month to treat his type 1 diabetes. At more than $300 per bottle along with required doctor’s appointments to maintain prescriptions and blood sugar testing supplies, the monthly expenses added up to several thousand dollars just to stay alive.
Alec would not have qualified for any of the patient-assistance programs offered by Novo Nordisk, Sanofi, or Eli Lilly because his income didn’t qualify as living below the poverty line.
These are just a few of the hoops a person with diabetes must jump through to demonstrate eligibility for these programs.
Had his parents known he was struggling, they would’ve helped him in a heartbeat, but as a newly independent young man, Alec tried to manage the financial burdens of type 1 diabetes on his own.
“Because he’d only had type 1 diabetes for two years and had likely just finished that honeymoon phase [during which your pancreas is still producing some insulin],” explained Smith-Holt, “I think he just did not realize that cutting back his insulin that much was going to become so dangerous so quickly.”
In 2018, Smith-Holt, her husband, and other advocates from #insulin4all began working in Minnesota to pass the Alec Smith Affordable Insulin Bill. If passed, this bill would provide a patient with any type of diabetes a 30-day supply after filling out a short application attesting that they cannot afford the out-of-pocket expenses of the insulin they need in order to stay alive — whether or not they have insulin.
It took two years of showing up over and over and over in court, meeting with the governor and other lawmakers who were all heavily influenced and lobbied by representatives for Novo Nordisk, Sanofi, and Eli Lilly.
“Prior to #insulin4all showing up at the Minnesota capital and working that first year to get the bill passed, there were very few pharmaceutical lobbyists in Minnesota,” explained Smith-Holt.
“As soon as they were aware of Alec’s bill, we started to notice these lobbyists were showing up in full force, representing every major manufacturer of insulin, meeting with legislators to prevent the bill from passing.”
Smith-Holt recalls one week of working to pass the bill when its success felt imminent.
“And then, all of a sudden, the bill just disappeared. Something happened behind closed doors between legislators and BigPharma’s lobbyists that influenced the decision.”
But Smith-Holt, her husband, and the army of #insulin4all advocates didn’t give up — and Novo Nordisk, Sanofi, and Eli Lilly continued to fight at every opportunity to prevent their efforts to make insulin more accessible and more affordable to the people who depend on it to stay alive.
“During year two, every single time we testified, a lobbyist from one of those ‘big 3’ were there to testify,” explains Smith-Holt. “Their lobbying dollars had doubled in Minnesota in order to come back at us in full force. All three of these insulin manufacturers were writing letters to every legislator involved in potentially passing the bill.”
All three insulin manufacturers were calling the author of the Alec Smith Affordable Insulin Bill asking for special meetings, including their top executives.
Smith-Holt sat in on just one of those meetings, listening to Novo Nordisk and Eli Lilly saying they already offer patient assistance programs and offered to simply change the wording on their website or tweaking their programs just slightly here and there.
Smith-Holt and other #insulin4all advocates said no.
“It’s not enough,” said Smith-Holt. “There’s no law forcing them to maintain these programs. They can simply drop them a few months from now.”
Finally, in the Spring of 2020, Smith-Holt, her husband, and their fellow #insulin4all advocates celebrated their success when Minnesota legislators passed the Alec Smith Affordable Insulin Bill. While devastatingly too late for Alec, this groundbreaking stride offers the potential to save thousands of lives for years to come in the state of Minnesota.
But these advocates know this isn’t enough, and Novo Nordisk, Sanofi, and Eli Lilly are still choosing profits over the lives of the patients who depend on insulin to survive.
Will BigPharma be held accountable for price-gouging?
“The solution to the insulin pricing crisis fundamentally has to happen on the federal level,” said Tsaplina, who was the Strategy and Action Lead for the New York #insulin4all chapter through April of this year. “T1international state chapters can work on important stop-gap solutions to help bring relief to some families to ensure people get the insulin they need to live, but this isn’t a replacement for national legislation, and doesn’t cover everyone who needs insulin to live.”
Tsaplina points out many flaws in the patient assistance programs touted by Novo Nordisk, Eli Lilly, and Sanofi:
What about patients in low-income environments who cannot afford or don’t have access to a stable internet? Those who receive very little diabetes education and support, and do not know about these programs?
For a patient rationing insulin and enduring daily high blood sugars, how are they expected to have the energy and mental clarity and stamina required to jump through the series of hoops that might eventually lead them to get some version of “patient assistance” in programs that are designed to serve as few people as possible?
Organizations intended to advocate for the benefit of patients with diabetes — the American Diabetes Association and the JDRF — rely heavily on funding from these pharmaceutical giants and have made zero effort to support lowering the list price of insulin. (They, however, tried taking credit for the work of #insulin4all.)
“To date,” explained Tsaplina, “they have lacked meaningful advocacy that supports solutions to permanently lower the list price of insulin so we don’t lose another life to insulin rationing.”
At the end of the day, these patient assistance programs and insulin copay price-caps are an effort to make it seem as though they are doing something when in fact they are still profiting wildly.
Tsaplina, Smith-Holt, and their fellow advocates at #insulin4all aren’t satisfied and continue to fight, for example, for a “comprehensive insulin package” in NY State that would address the criminal actions on the price of insulin in the United States.
Tsaplina said it best when she asked, “Why on earth should we be satisfied with coupons when insulin costs $30 per vial in Canada?”
New CMS $35 Monthly Cap Plan
On May 26, 2020, the Centers for Medicare & Medicaid Services (CMS) announced a Senior Savings Model in which insulin copays will be capped at $35/month beginning in 2021.
Over 1,750 standalone Medicare Part D plans & Medicare Advantage plans with prescription drug coverage have applied to participate in Part D Senior Savings Model, offering coverage in all 50 states, DC, and Puerto Rico.
This is a step in the right direction but important details to be determined include:
Source: Juliette Cubanski (Twitter) of the Kaiser Family Foundation (website)
- What will be the monthly premiums for participating Part D enhanced plans in 2021 relative to other enhanced plans and basic plans?
- Currently, enhanced plan premiums are roughly twice the level of premiums for basic plans, on average
- Insulin manufacturers seem to bear much of the cost of this enhanced benefit through the 70% coverage gap discount
- Plan sponsors were offered additional financial protection through a narrower risk corridor, and costs can be passed on to enrollees in the form of higher premiums
- How many insulin products does each participating Part D plan actually offer at the $35 flat copay? Plans don’t have to cover every insulin product at $35/month, just one of each dosage form (vial, pen) and type (e.g., long-acting, rapid-acting).
- Part D enrollees may have to switch plans (from basic to enhanced or from one enhanced plan to another) and/or switch insulin products in order to see these savings.