Mending Metabolism
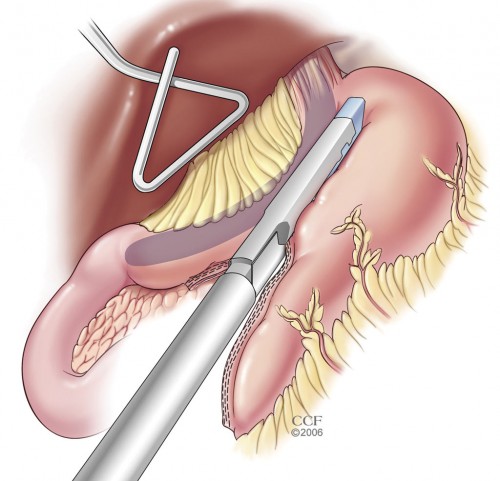
A new Cleveland Clinic study of metabolic outcomes, including diabetes remission, in patients who underwent bariatric surgery between 2004 and 2007, suggests that sooner is better than later when choosing one of the three common procedures – gastric bypass, sleeve gastrectomy, or gastric banding. The study, conducted and reported on by Dr. Stacy Brethauer and a team of 8 other Cleveland Clinic physicians, also points to regaining weight, and the length of time a patient had suffered from poorly controlled diabetes before surgery, as significant factors in diabetes recurrence.
Frequent visitors to Insulin Nation are already familiar with the positive, at times spectacular, outcomes possible as a result of gastric bypass (Operating on Diabetes and Resurrecting The Pancreas). But only 1% to 2% of people with Type 2 diabetes who are eligible for a bariatric procedure have one performed. If there is a single, most important takeaway from the study results, Dr. Brethauer says, it is that sooner is better than later. Bariatric surgery early in the course of a patient’s diabetes is far more likely to produce remission, and sustained improvements in blood pressure and cholesterol levels, than the same procedure performed as a “last resort.”

The latest research studies a group of 217 patients, almost three-quarters of them women, who had a bariatric procedure at Cleveland Clinic between 5 and 9 years ago. 75% of these women received a gastric bypass, while the other 25% had either sleeve gastrectomy or adjustable gastric banding surgery. The average time with diabetes prior to surgery ranged from 5 to 16 years. Pre-operation, all subjects had an A1c of 7.4% to 7.6%, while between 75% and 81% had high blood pressure and more than 90% had high LDL, or “bad,” cholesterol. Sadly, the blood pressure and cholesterol readings are in line with national averages; only 18% of people with diabetes achieve healthy levels of each, along with an ADA-recommended A1c of 7.0% or less.
It isn’t hard to identify the culprit lurking behind these poor numbers: excess weight. While the threshold for bariatric surgery qualification is a BMI of 35 or higher, these women, with an average BMI of 49, were morbidly obese. A BMI of 49 is equivalent to a height of 5’4” (the U.S. average for all women) and a weight of 285 lbs. Combining diabetes with this much weight and corresponding elevated blood pressure and bad cholesterol meant that these women were on the road to serious complications, including heart disease, kidney failure, and potentially blindness and amputations.
So, what results did the surgeries produce? In 162 subjects who received a gastric bypass, weight loss after 6 years averaged 60.5 lbs., almost 25% of pre-surgery body weight. Sleeve gastrectomy subjects lost an average of 49.5 lbs, or 25%, and gastric band patients lost 29.5 lbs. on average, about 23% of their weight going in. A1c percentages for the bypass and gastrectomy subjects remained below the ADA-recommended level of 7.0% at 6 years, while the average decline for banding patients was slightly more than a full percentage point, but still somewhat higher than 7.0%. Almost as significant as diabetes remission, key body metabolic components showed dramatic improvement. Blood pressure in most subjects dropped significantly, to less than the ADA recommended level, and LDL cholesterol also fell significantly below the guidelines. Weight loss and maintaining the new weight are directly correlated to these improvements.
 The results make it appear that gastric bypass is the preferred option, but that isn’t necessarily true. Gastric sleeve and gastric banding surgeries have shown marked success in eliminating diabetes in other studies, but almost all of the patients who underwent either of these procedures in the Cleveland Clinic study were older, had experienced poorly controlled diabetes for longer than the other patients, or had other factors that ruled out a bypass procedure.
The results make it appear that gastric bypass is the preferred option, but that isn’t necessarily true. Gastric sleeve and gastric banding surgeries have shown marked success in eliminating diabetes in other studies, but almost all of the patients who underwent either of these procedures in the Cleveland Clinic study were older, had experienced poorly controlled diabetes for longer than the other patients, or had other factors that ruled out a bypass procedure.
Most important, 61% of the bypass recipients achieved full or partial remission of diabetes six years after the surgery, while an additional 31% significantly improved their metabolic profile. With this level of longer-term success, it is surprising that more people with Type 2 diabetes and serious weight issues don’t opt for one of the bariatric procedures. Dr. Brethauer and many of his colleagues believe it is a combination of misplaced fears about the dangers of bariatric surgery, a lack of understanding of potential benefits by the primary care physicians who provide the majority of Type 2 diabetes care, and slow-to-adjust insurance reimbursement that fails to take into account the financial benefits of well-controlled or eliminated diabetes across many years of better health by those who elect one of the surgeries.
Why does diabetes return in some patients? The study results point to regained weight as a primary factor as well as the duration of diabetes prior to surgery. While you might think that reducing your stomach to a capacity of 1 to 5 ounces of food at any one time makes it impossible to gain weight, bariatric surgery patients can put on the pounds years after surgery if high carbohydrate foods are consumed instead of high protein foods, and if patients fail to maintain an active lifestyle. Even so, it appears that bariatric surgeries can dramatically alter the metabolic profile in just about anyone, and this alone is an “ounce of prevention equals a pound of cure” scenario for people who find dealing with diabetes and excess weight to be too much to handle without help.







