Diabetes-Related Distress Leads to Higher A1C Scores
Sometimes, studies must prove what people with Type 1 diabetes often already know from experience. That was the case of a recent study which revealed a connection between elevated A1C scores and diabetes-related distress in people with Type 1 diabetes.
According to a report in Diabetes Medicine, researchers with the University of California San Francisco and other diabetes-focused research and behavioral institutes determined that people with Type 1 diabetes experiencing elevated diabetes-related distress were more likely to be at risk of missing insulin boluses or having worsening glycemic control.
The study sampled 224 people with Type 1 diabetes. Data was collected over a nine-month period through online surveys and telephone calls to patients by study psychiatrists. It’s important to note that study participants consisted mainly of well-educated patients from Northern California and Canada with a high rate of computer accessibility and access to healthcare; this sample group’s demographics might limit how much we can extrapolate the findings for the Type 1 population in total.
While the study’s results showed a significant relationship between distress and A1C levels, researchers have yet to discover the root cause for the relationship between the two. Findings suggest a chicken-or-the-egg scenario: a negative change in distress occurs with negative changes in A1C, and vice versa. The two factors likely influence each other cyclically over time. As distress levels increase, so, too, does the likelihood of missing insulin boluses, being less physically active, and making less healthy decisions in diet management. This increases the risk of more frequent episodes of hypoglycemia and diabetic ketoacidosis, which of course results in more stressful situations in diabetes management.
Read more: Measuring Parental Distress of a Type 1 Diagnosis
Researchers also found that when participants don’t receive timely and quality follow-up care from their healthcare providers, they are more likely to suffer from diabetes distress. Researchers suggest that this finding should empower doctors and healthcare providers to implement intervention methods to help break the cycle.
Dr. Mark Heyman, a diabetes psychologist, person with Type 1 diabetes, and founder and director of the Center for Diabetes and Mental Health, was asked about the findings. He said supporting the mental health of a person with Type 1 diabetes is crucial in managing the condition.
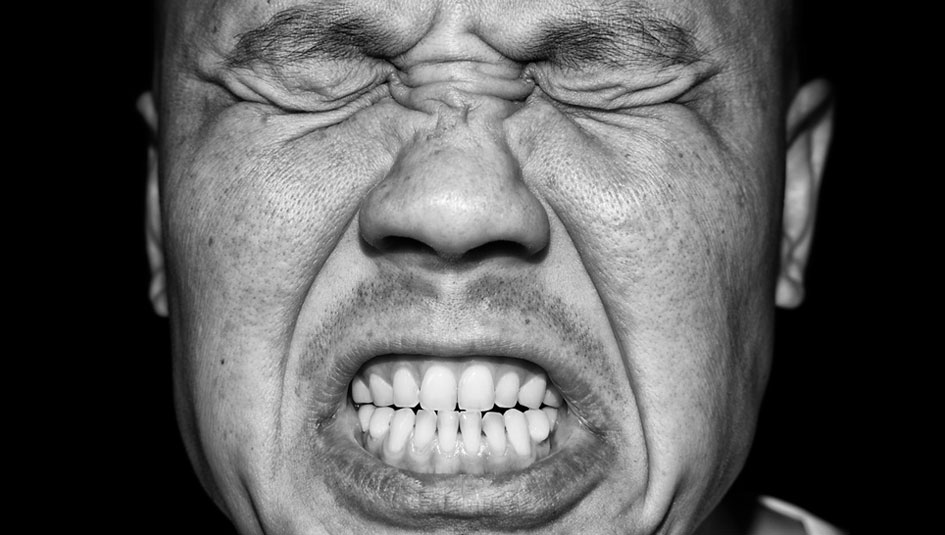
“People with Type 1 diabetes are more prone to psychosocial challenges. The daily grind of Type 1 diabetes is nonstop. It can get frustrating and people can get angry and begin to feel hopeless,” he said. “The goal is behavioral change and helping people see that yes, it is a lot of work, but if you’re willing to do it, the benefits far outway the costs.”
Read Dr. Heyman’s column: Should You Go to a Diabetes Psychologist?
The study shows that diabetes distress will not improve on its own without intervention. Dr. Heyman shares how he motivates patients who are dealing with diabetes distress.
“You have to take a step back first and help people understand why taking care of themselves is important,” he said. “For example, rather than just saying, ‘I want to live a long, healthy life,’ patients find more success when they have specific goals such as, ‘I want to manage my diabetes so I can have a child some day and watch them go to kindergarten.’”
He has his patients pick one near-term goal or action to focus on that will have the biggest impact on their immediate lives. For example, a patient in high school would skip boluses during school days; not surprisingly, she struggled with high glucose readings. Rather than focusing on the meta-goal of lowering her glucose levels overall, she set an immediate goal of taking her insulin every day to cover school lunch. She worked with Dr. Heyman to take note of how her energy and pain improved once she did this. Eventually, bolusing for lunch at school became routine and she was able to improve control of her blood sugars.
The American Diabetes Association maintains a directory of diabetes-focused mental health providers. You can access that list by clicking here.
Thanks for reading this Insulin Nation article. Want more Type 1 news? Subscribe here.
Have Type 2 diabetes or know someone who does? Try Type 2 Nation, our sister publication.







