I was more than four years into my diabetic journey before I finally asked my endocrinologist to help me start the process of getting an insulin pump. We had discussed it in passing before, but my numbers were so strong on my current routine of multiple daily injections (MDI) that pump therapy seemed unnecessary. But for me, the time had finally come to make the leap.
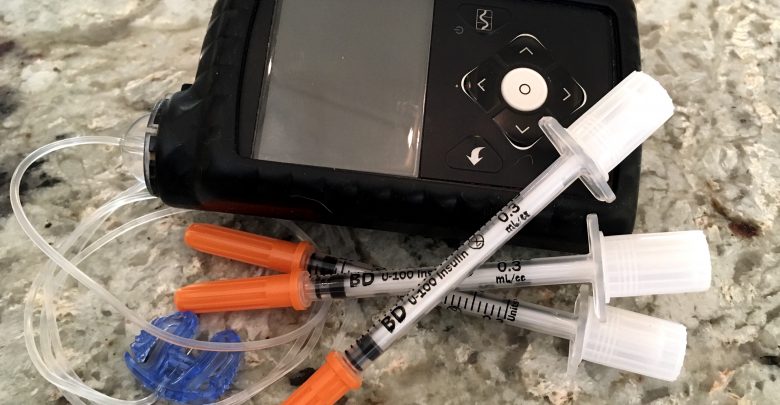
The transition to an insulin pump was a little tougher than I anticipated. In addition to the insurance headaches (nothing like receiving an unexpected bill for $14,000 dollars!) and the arduous training sessions with the pump manufacturer, I also had to get used to having something attached to me at all times.
Insulin pumps can be a little clingy, it turns out.
But looking back, I’m glad I finally made the decision, even if the pump itself wasn’t actually what I was after.
I Really Wanted the CGM
What convinced me to ask my doctor about a pump that day wasn’t actually a desire to give up MDI. I didn’t really mind injections, other than occasionally forgetting my long-term insulin pen during poorly timed outings. But otherwise, I was doing well. My A1Cs were consistently in the 6’s and I had a strong understanding of how to manage my diabetes using a combination of short- and long-term insulin pens.
What I was interested in, was getting a continuous glucose monitor (CGM). I loved the idea of being able to check in on my blood sugars simply by glancing down at a screen. No more having to set alarms to remind me to meter two hours after eating. And no more surprises when the meter returned a reading in the high triple digits. I could watch my blood sugars rise and fall in real time on a graph with loads of valuable information.
Unfortunately, at the time, getting a standalone CGM meant always carrying around a receiver. I knew that eventually I would want to switch to an insulin pump and having to juggle both a pump and a receiver seemed like more than I could handle. Up until my diagnosis, I had never even owned a purse. Carrying around snacks, glucose tabs, and insulin was already a bulky load.

For me, the Medtronic combined pump and CGM seemed like the best way to go. I’d get the CGM I wanted and deal with switching to a pump a little earlier than planned. With my doctor’s approval, I was ready to learn how to manage my diabetes in a whole new way.
Insulin Pumps are Not Without Complications
One of the reasons my doctor rarely brought up pump therapy is because of the extra complications it can add to a diabetic’s life. It seems counterintuitive. After all, this is a high-tech gadget that has saved a ton of lives.
But all those benefits don’t come without some drawbacks.
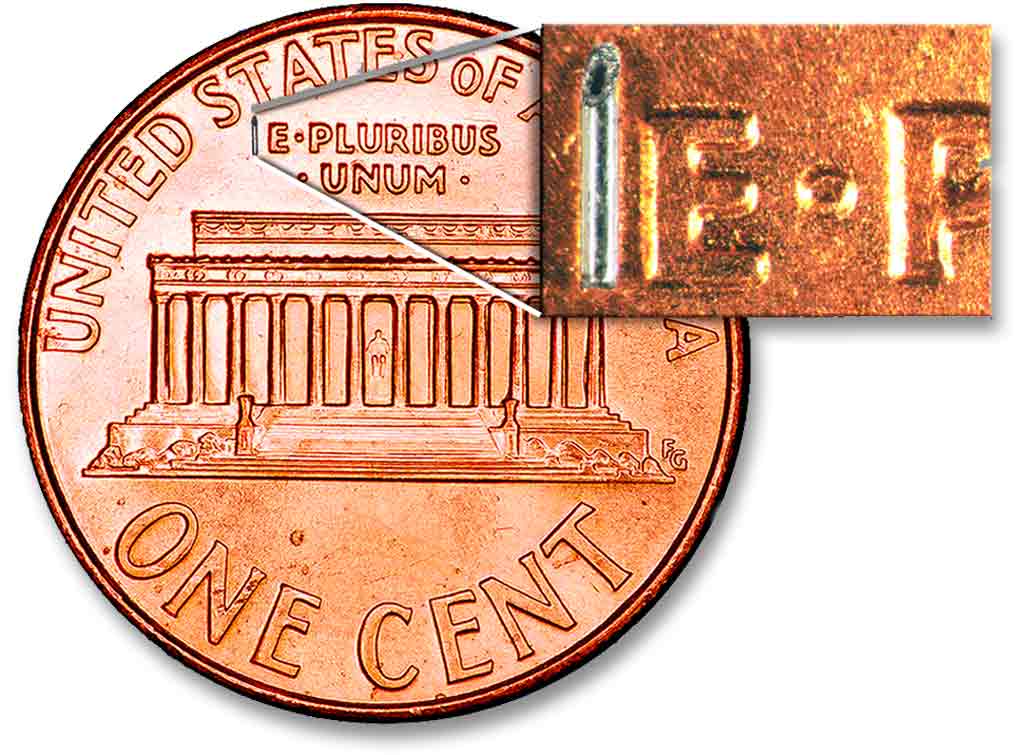
Injections are simple. You calculate how much insulin you need. You stab yourself in some flabby area of your body. And, if your blood sugar doesn’t respond the way you wanted it to, you know your calculations were either wrong or you need to reconfigure your carb or basal equations. If you’re unlucky, maybe occasionally a vial of bad insulin will send your numbers into chaos, but that’s really all the confusion you have to worry about.
Pumps, on the other hand, can cause blood sugar chaos on multiple fronts. If your numbers dip or peak unexpectedly, it could be a carb ratio or basal rate problem (on the plus side, at least you know the math is correct). Or, it could be an air bubble in your tubing. Or a bad site. Or maybe you sat in the sun too long and the insulin in your reservoir has gone sour. Or maybe the pump is malfunctioning (probably not, but your mind always goes there). Or maybe your cat kneaded a hole in your tubes and insulin has been leaking out for hours.
All these possible explanations mean a lot of extra considerations on your part. And this is all in addition to the steep learning curve that comes with starting pump therapy.
The Benefits of Insulin Pump Therapy
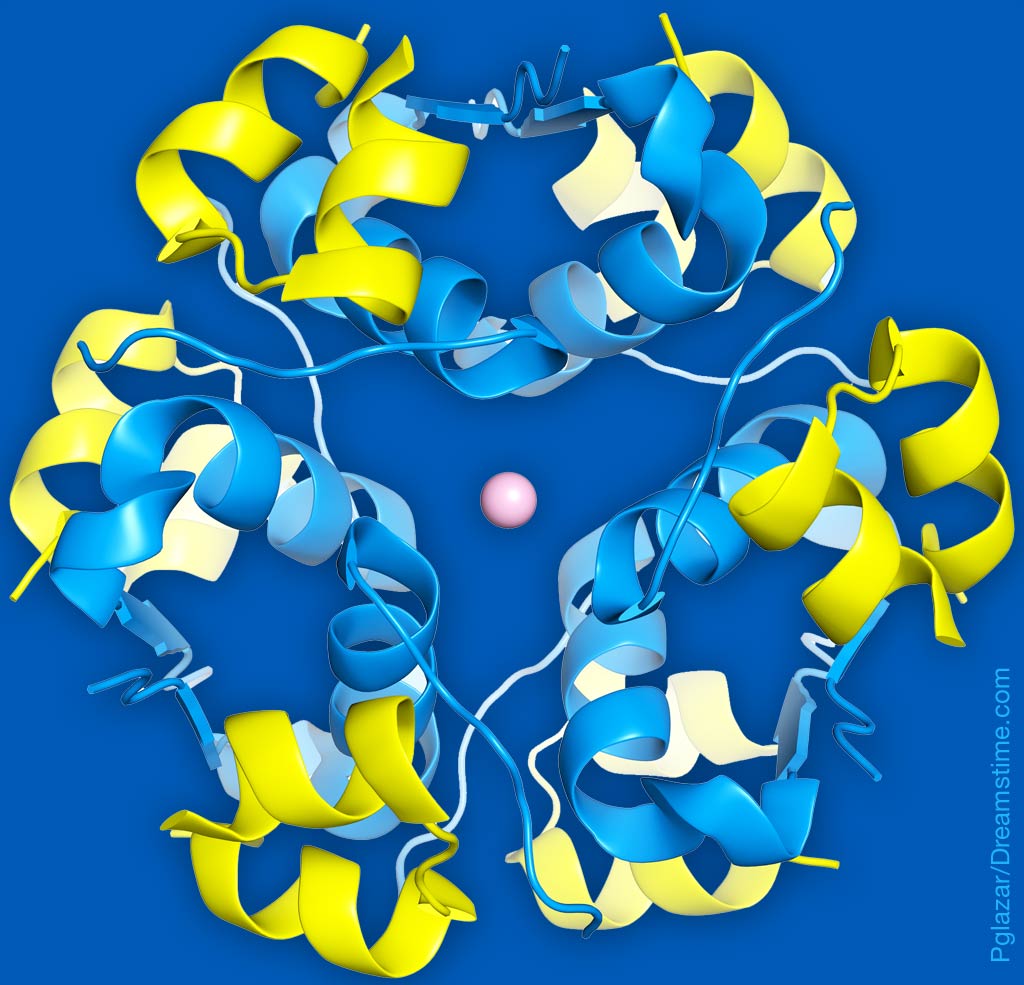
But there are some serious benefits, too. When I was on MDI, I’d take one flat rate of long-acting insulin to cover me throughout the day. That meant I’d be working off basically the same basal rate of insulin every hour. What I discovered when I switched to the pump, was that my basal insulin needs change drastically throughout the day. For a period in the morning, I need almost no basal insulin at all. While in the afternoon I need almost a full unit each hour.
Having a pump gives me the unique ability to calculate my insulin needs at any given moment down to a tiny fraction of a unit. This leads to way better control overall. For me, this highly flexible, super-individualized treatment approach is worth any added complications.
And did I mention it also saves me from having to do math?
Not Looking Back
A lot has changed since I first switched from MDI to pump therapy. If I was making that switch today, I would have the option to get a standalone CGM that works with my phone or smartwatch. And maybe, that would have meant I never switched to a pump at all.
But as things are, I have been a pump user for over six years. While it does still cause the occasional headache (like getting my tubing caught on drawer handles, doorknobs, and seatbelts), it has provided loads more in benefits. And those benefits show in the form of lower A1C’s and a lot of pretty, flat lines on my CGM.