Supportive Coworkers Positively Impact Blood Glucose Activity

Individuals living with Type 1 diabetes know that blood sugar ups and downs are common even for those who follow scrupulous routines. In the professional world, these high and low blood sugars are public. There are deadlines, workflows, and priorities that do not stop for diabetes. There are meetings and presentations, during which a blood sugar check can feel uncomfortable. But these realities do not mean that diabetes-related tasks are unwarranted.
My diabetes care is essential to my productivity in the workplace. When I have high blood sugar, my brain feels “fuzzy,” and it takes me a little bit longer to do normal tasks like writing emails and prioritizing tasks. Low blood sugars also slow me down, since they often require intervention. I’ve often wondered about the effects of these delays on my productivity.
One study published in 2011 investigated the impact of non-severe hypoglycemic events on work productivity and diabetes management using an online survey for individuals with diabetes from the United States, the United Kingdom, and France. The researchers defined “non-specific hypoglycemia events” or NSHEs as a low blood sugar for which the person with diabetes needed help from other individuals. This study found that hypoglycemic events have a significant impact on productivity, and it indicated that fine-tuning treatments may have a positive effect on both the individual with diabetes and the workplace as a whole.
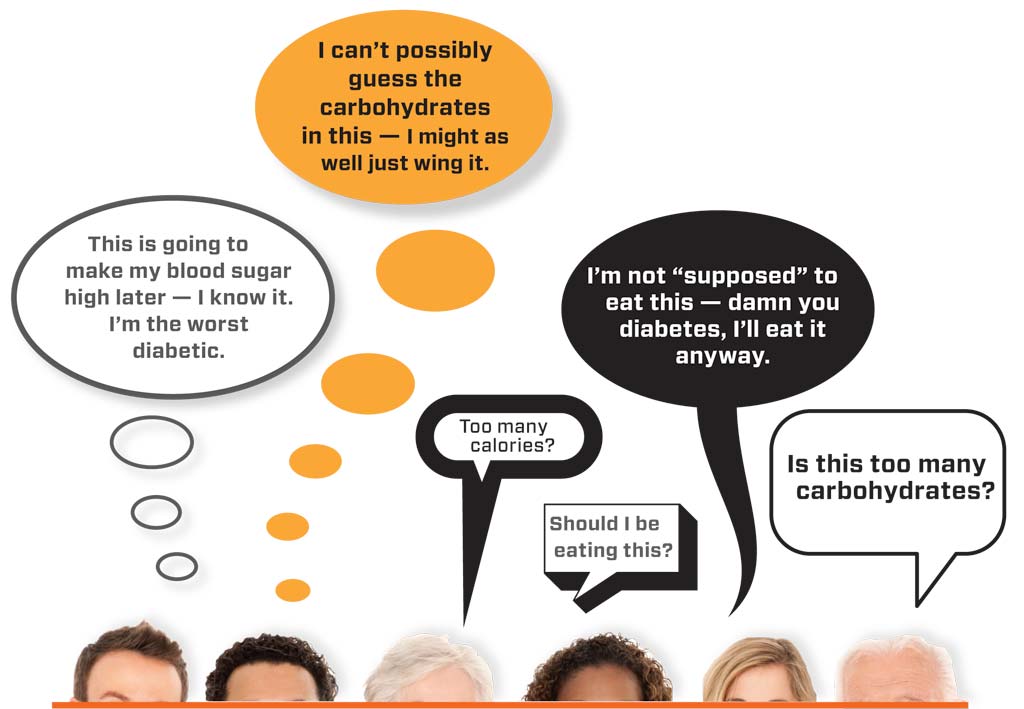
These findings make sense. Of course hypoglycemic events affect productivity! But they led me to additional questions: what factors in the workplace could make these hypoglycemic events more manageable? And what would cause them to occur less frequently? I suspected that increased comfort to test blood sugars and give insulin injections could lead to less frequent hyperglycemic and hypoglycemic events.
This idea is suggested by a study published by the American Diabetes Association, which analyzed how a group of 129 insulin-dependent diabetics cope with diabetes at work. The study found that the work itself did not impact glycemic control; rather, glycemic control was influenced by psychosocial adaptations. Individuals with involved coworkers and supportive supervisors fared better.
In my first job out of college, I worked in a diabetes management program at a federally qualified health center. Not only were my colleagues aware of my diabetes, they were interested and engaged, always wanting to know more about my condition. In that environment, my A1C significantly improved.
But during this time, I realized that my positive experiences were not shared by all. I worked with migrant farmworkers with diabetes who spent long hours in an apple packing shed or in the field picking pears and cherries. Many times, I heard these individuals say that there was no time to eat or test blood sugar. This was because, each day, their success depended on their productivity—the quantity of fruit picked.
I often told these farmworkers that it’s okay to share about diabetes. In fact, being more upfront about some of the daily struggles may help to create an environment in which coworkers are more involved, leading to better management during the work day. Understandably, individuals are reluctant to open up about diabetes on the job. But the reality is that both types of diabetes are becoming increasingly common in the workplace. So, chances are, there are others with similar needs.
Do you have an idea you would like to write about for Insulin Nation? Send your pitch to submissions@insulinnation.com.
Thanks for reading this Insulin Nation article. Want more Type 1 news? Subscribe here.