Faster Insulin: Extracellular Action
Until we find a biological cure for diabetes, help transplanted islets survive and thrive, or discover how to regenerate normal insulin secretion in a pancreas whose beta cells have been ravaged by auto-immune attack, the best science and technology can do is develop ways to make man-made insulin act more like its naturally produced counterpart. The most promising developments today revolve around increasing the speed of insulin absorption and shortening its “tail,” the time it spends in our bodies at elevated levels. Insulin Nation has covered various approaches to faster insulin, including Mannkind’s Afrezza® inhalable insulin therapy [Inhalable Insulin: A Breathtaking Development], heating the area around infusion or injection sites [Faster Insulin: A Heated Exchange], or intradermal injections using super-short needles [Faster Insulin: Short and Sweet].
Another company closing in on improving the speed of insulin action is Halozyme Therapeutics, (www.halozyme.com) a biopharmaceutical developer located in San Diego. Halozyme focuses on human enzymes that temporarily alter a specific component of the extracellular matrix (ECM), the “glue” that holds all our cells and connects them to tissues. Hylenex®, one of the company’s products, is currently being tested in Phase IV clinical trials in combination with rapid-onset insulins to make pre-meal bolus insulin work faster and disappear more quickly from the body.
Hylenex® is a purified preparation of the enzyme recombinant human hyaluronidase (rHuPH20). Previous clinical trials conducted by Halozyme have demonstrated that formulating the rHuPH20 enzyme with insulin or administering it before a bolus dose alters insulin profiles to become more like those found in people who don’t have diabetes. So, how does rHuPH20 work, and what does it do?
Opening Paths Through A Forest Of Skin

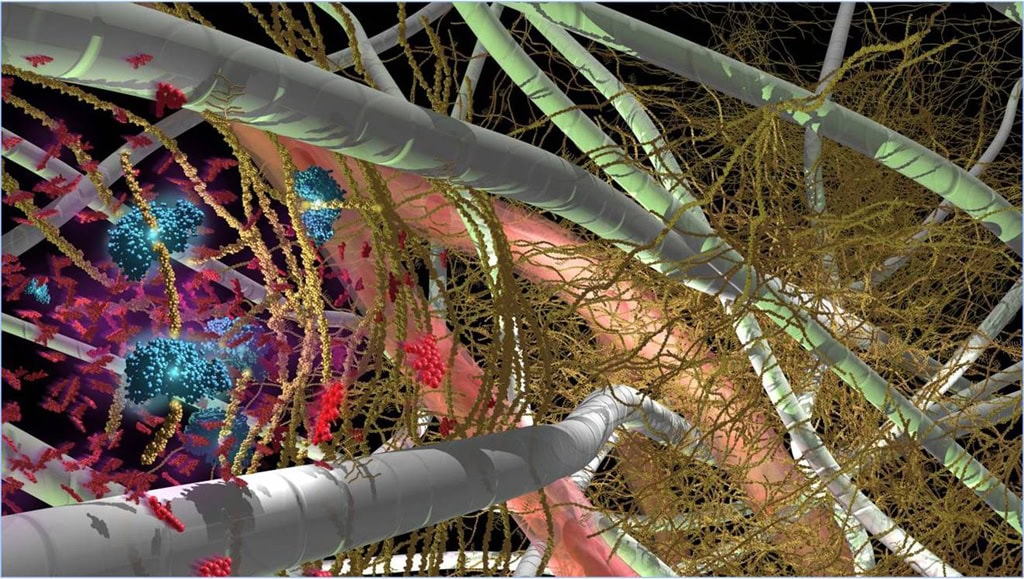
If you struggled through the previous description, here is a simplified version of what rHuPH20 does. Imagine that the area just below your skin surface is like a forest, full of trees and bushes.. Hyaluronan, a short lived substance in the skin, is like the bushes between the trees; other proteins in the skin like collagen would be the trees thenselves. Halozyme’s lead enzyme, rHuPH20, temporarily opens small paths through the forest by degrading hyaluronan, which is like trimming the bushes. With the “forest” floor now more accessible, a co-injected drug, like insulin, reaches its targets more easily, is dispersed over a greater surface area, and gets absorbed into the capillary beds more quickly. As a result, traditional subcutaneous delivery of insulin, either by injection or infusion, occurs more quickly.
Unlike trees or bushes exposed to defoliants, however, the bushes– hyaluronan – grow back very quickly. Within 24-48 hours, the structure of the skin returns to what it was before treatment. The rebirth is not miraculous; the average 155 lb. person has about 15 grams of hyaluronan in their body, and a third of it is degraded and synthesized every day of their lives. The novelty of Halozyme’s approach is marrying the properties of recombinant hyaluronidase to various drug therapies.
Initially, Halozyme focused on using rHuPH20 to create ways to change intravenous therapies to subcutaneous solutions. Subcutaneous injections may be preferable to intravenous drug delivery (IV) for many reasons, not the least of which is patient comfort. But, a challenge to switching from IV to subcutaneous therapy is that some of the drug gets caught up in the skin tissue, and only a portion of it actually gets absorbed into the body. Halozyme’s technology is intended to offer a solution to this problem, by temporarily speeding up drug absorption as described above. The company has current partnerships focusing on more effective drug absorption based on its rHuPH20 technology with Roche, Baxter U.S., ViroPharma, and Pfizer. In each case, the enzyme rHuPH20 may help make the switch from IV to subcutaneous therapies easier.
Analog Insulin: A Promise Half-Fulfilled?
The original concept behind analog, or rapid-onset, insulin, was replacing a dose of regular insulin that needed to be injected a half-hour or more before a meal. The thought was that you could take the faster onset insulin just before eating, which appealed to many people because it gave them a measure of control in an unpredictable world, where mealtimes don’t always conform to a rigid schedule. Rapid-onset insulin was seen as a great success, because it did demonstrate better after-meal glucose control when compared to regular insulin injected before eating..
Then continuous glucose monitors entered the picture, and they revealed a problem to patients and doctors alike. According to Dr. Jay Skyler, Professor of Medicine, Pediatrics and Psychology at the University of Miami Miller School of Medicine, “patients could see that rapid-acting insulin analogs were still not rapid enough. If you had a high carbohydrate meal, at a half hour, 1 hour, or 1.5 hours, you saw significant elevations in glucose levels. The rapid-acting insulin analog wasn’t peaking until after the meal did.”
In this context, it isn’t surprising that, Halozyme identified insulin as an opportunity for improving current diabetes therapies. The large molecules of rapid onset insulin take time to break down into smaller particles that can penetrate the extracellular matrix and then be absorbed into the bloodstream. This is one of the reasons that rapid onset insulin does not work as quickly as its naturally secreted counterpart. Halozyme has attempted to address that challenge by focusing not on the molecular structure of insulin, as others have, but on the structure of tissue. By temporarily degrading hyaluronan, insulin administered with rHuPH20 is absorbed more quickly. The enzyme has been clinically tested in trials with all rapid analog insulins currently sold in the U.S.
Coformulation: Adding A “Special Ingredient”

There are two ways rHuPH20 can be used to produce faster rapid onset insulin. One approach is co-formulation with insulins before it is injected.
“In some of our earlier clinical studies, we tested rHuPH20 formulated with insulin analogs,” says Dr. Gregory Frost, co-founder of Halozyme and its CEO. “In these trials, the injected insulin was clearly absorbed faster. These studies also suggested the glucose levels weren’t spiking as high after meals because the insulin was getting in faster, in time to deal with the glucose load of the meal.”
Physicians who have also tested rHuPH20 formulated with insulin concur. “The concept was to use hyaluronidase (rHuPH20, the active ingredient in Hylenex®) to increase the rate of absorption by creating a coformulation with insulin,” says Dr. Skyler, “That’s the study that my colleagues and I did. The coformulation did exactly what it was supposed to do. The insulin worked faster,” he reports. Halozyme is continuing to explore these coformulation studies, which must go through the entire FDA approval process because the mixtures constitute a new drug with the insulin and enzyme formulated together.
A “Killer App” For Pumps?
The other way to use rHuPH20 is pre-administration of the enzyme by itself using insulin pumps. The concept is to infuse just a single dose of Hylenex® (an FDA approved formulation of the enzyme alone) when pump patients change infusion sites every two to three days. Halozyme is currently enrolling trial subjects in a Phase IV trial to further observe the effect of Hylenex® on insulin absorption, along with other results that include a variety of endpoints: A1C, postprandial glucose, and rates of hypoglycemia all will be studied and reported on.
Earlier clinical trials conducted with pump patients showed another equally promising observation and important result: a consistency of insulin absorption over the three days between infusion site changes if rHuPH20 was given to subjects before they began to pump again. “The patients received a single dose of rHuPH20 upfront and then wore the pump as they normally do,” says Frost. “What we saw in these clinical trials was that the insulin absorption profile on day 3 was very similar to the insulin absorption profile on day 1. This might provide not only the ‘fast in and shorter duration’ of mealtime administration, but also more consistent insulin absorption every time you bolus. And that might offer a meaningful improvement for people who are on an insulin pump.”
Finally, in other clinical trials conducted by Halozyme, the insulin products formulated with rHuPH20 appeared to have a much shorter “tail,” or much less of a residual effect on glucose levels that may lead to hypoglycemic events, than current rapid-onset products. The shorter duration of insulin when combined with rHuPH20 might lead to fewer hypoglycemic events.
If all this turns out to be true, it would be good news for pump makers, who seem to need new evidence to stimulate infusion adoption among multiple daily injectors. Many who resist pump adoption report that they see injecting insulin as more convenient, even if the insulin action is more erratic. Tighter control combined with less risk of hypoglycemic events might be just the thing pump makers need to energize sales.
Creating Another “Aha” Moment
Halozyme’s work has attracted many advocates among leading professionals who specialize in diabetes. One is Dr. Daniel Einhorn, Medical Director of the Scripps Whittier Diabetes Institute and current President of the American College of Endocrinology. “When we first started using the analog insulin” he recalls, “it was very clear early to the first users, physicians, and nurses, that people were getting better postprandial control and fewer hypoglycemic episodes with these insulins. And patients felt better. But it took awhile – years – for that realization to hit the greater healthcare community. So what I would like to see with the ongoing Hylenex clinical trials is a reconfirmation of the ‘Aha’ experience, where using a faster, more predictable insulin enables you to gain better control.”
Dr. Einhorn also stresses the consultative nature of the current Hylenex® trials. “The scientists and researchers can do the best they can,” he says, “ but it is really the people with diabetes who are using pumps who are going to be the lead scientists to identify better therapies. This is a very live and very democratic process. With other disease states, the physician gives you something and the patient responds to it. With these patients, we’re looking to them to give us advice on how to best use this tool. So it is much more collaborative. I am very excited for that.”