5 Reasons People Ditch the Pump
Integrated Diabetes Services (IDS) provides detailed advice and coaching on diabetes management from certified diabetes educators and dieticians. Insulin Nation hosts a regular Q&A column from IDS that answers questions submitted from the Type 1 diabetes community.
Q – I see studies show that people with Type 1 do better on insulin pump therapy, but I sometimes hear of people stopping pump therapy to return to multiple daily injections. Can you tell me why it might be better for some people to stop using a pump?
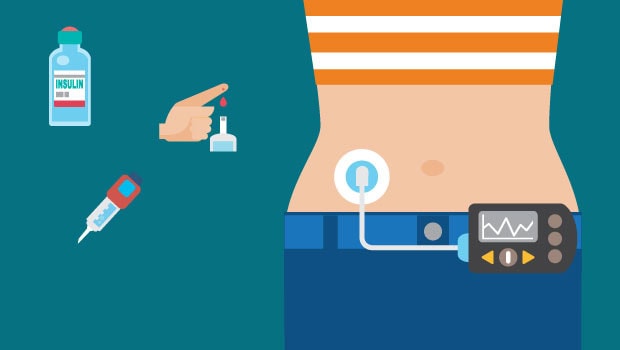
A – There are many more choices for insulin pumps than in the past, and many of these new pumps come with new and powerful technological options to help you with blood sugar management. Many clinicians promote pump use as the best way to achieve optimal control.
But is it really the end-all-be-all of diabetes management? As with everything in life, it comes down to personal choice and what works for you. It’s best to do your homework to evaluate if a pump is best for your lifestyle and blood sugar management needs.
There are plenty of articles discussing the pros of pump therapy, but few that discuss the cons. To offer some balance, here are some downsides to pump use that have caused people to switch back to multiple daily injections:
1) Mechanical Failure
Insulin pens and syringes don’t have mechanical parts – they will not malfunction or have errors. The more technology that is used to deliver insulin, the higher the chance that something can go wrong in a mechanical sense. It doesn’t happen often, but it does happen.
I have had several pump failures in 15 years of pump use; all were detected by the pump. Pump problems can include internal errors in the mechanics, air bubbles in the tubing, and kinks in the cannula. With pump therapy, diabetic ketoacidosis can set in if insulin delivery is interrupted and blood sugar levels aren’t being monitored.
2) Skin sensitivity
If you’ve used a pump in the past and have developed scar tissue or have skin sensitivity to the adhesive tape, it might prompt you to go back to injections. There are ways to avoid these problems, like adequately rotating the infusion site and employing barriers, but these don’t always work.
![]() 3) Visibility
3) Visibility
Diabetes is for the most part an invisible condition that we can hide, if we choose. With an insulin pump, it’s harder to hide. Also, being attached to the pump via tubing or pod is a 24/7 thing and for some this makes a pump a constant reminder of diabetes. This might be beneficial for some, but a psychological downer for others.
4) Expense
With pumps, cost is surely a consideration. Pumps and pump supplies cost significantly more than syringes and pens. Insurance companies vary in coverage, so the cost for out-of-pocket expenses might be what makes some turn back to the syringe.
If you can achieve the same level of blood sugar management and A1C scores without a pump, it may provide great savings. However, if you’ve done injections in the past, and can’t get your A1C below 7.0, you might want to consider the expense of an insulin pump worthwhile, as it could save you money down the road in prevented diabetes complications.
5) Personal Preference
A pump has the ability to fine-tune insulin doses down to the 0.025 unit, and that can make an enormous difference in control. Injections can only be delivered in 0.50 unit increments. This might mean you have to take a lot of little injections throughout the day, but some people like that kind of hands-on approach, and don’t mind the amount of effort it takes to achieve good blood glucose control.
The important thing is to take the time to explore the options available and see what works for you. Get the pros and cons to all the pumps on the market; we came up with a list that you can access here. If possible, work with a certified diabetes educator to road-test an insulin pump. While insulin therapy is not optional for people with Type 1, any option for achieving good blood glucose control should fit your lifestyle and needs.
Integrated Diabetes Services provides one-on-one education and glucose regulation for people who use insulin. Diabetes “coaching” services are available in-person and remotely via phone and online for children and adults. Integrated Diabetes Services offers specialized services for insulin pump and continuous glucose monitor users, athletes, pregnancy & Type 1 diabetes, and those with Type 2 diabetes who require insulin. For more information, call 1-610-642-6055, go to integrateddiabetes.com or write info@integrateddiabetes.com.
Thanks for reading this Insulin Nation article. Want more Type 1 news? Subscribe here.
Have Type 2 diabetes or know someone who does? Try Type 2 Nation, our sister publication.